预约演示
更新于:2025-05-07
RECK
更新于:2025-05-07
基本信息
别名 hRECK、RECK、reversion inducing cysteine rich protein with kazal motifs + [3] |
简介 Functions together with ADGRA2 to enable brain endothelial cells to selectively respond to Wnt7 signals (WNT7A or WNT7B) (PubMed:28289266, PubMed:30026314). Plays a key role in Wnt7-specific responses: required for central nervous system (CNS) angiogenesis and blood-brain barrier regulation (By similarity). Acts as a Wnt7-specific coactivator of canonical Wnt signaling by decoding Wnt ligands: acts by interacting specifically with the disordered linker region of Wnt7, thereby conferring ligand selectivity for Wnt7 (PubMed:30026314). ADGRA2 is then required to deliver RECK-bound Wnt7 to frizzled by assembling a higher-order RECK-ADGRA2-Fzd-LRP5-LRP6 complex (PubMed:30026314). Also acts as a serine protease inhibitor: negatively regulates matrix metalloproteinase-9 (MMP9) by suppressing MMP9 secretion and by direct inhibition of its enzymatic activity (PubMed:18194466, PubMed:9789069). Also inhibits metalloproteinase activity of MMP2 and MMP14 (MT1-MMP) (PubMed:9789069). |
关联
100 项与 RECK 相关的临床结果
登录后查看更多信息
100 项与 RECK 相关的转化医学
登录后查看更多信息
0 项与 RECK 相关的专利(医药)
登录后查看更多信息
718
项与 RECK 相关的文献(医药)2025-05-01·The Spine Journal
Ropivacaine-epinephrine-clonidine-ketorolac is an effective opioid-sparing local anesthetic for patients undergoing posterior spinal fusion
Article
作者: Rahm, Mark D ; Soto, Jose M ; Keith, Kristin A ; Lyon, Kristopher A ; Nguyen, Anthony V ; Huang, Jason H
2025-03-01·International Journal of Medical Microbiology
Nasopharyngeal carriage of Staphylococcus aureus in a rural population, Sierra Leone
Article
作者: Rudolf, Viktoria ; Sesay, Maxwell ; Theiler, Tom ; Sesay, Desmond Mohamed ; Mellmann, Alexander ; Schaumburg, Frieder ; Grobusch, Martin P ; Grebe, Tobias ; Kleine, Lisa Maria ; Kanu, Emmanuel Marx ; Loismann, Henning ; Kalkman, Laura C
2025-03-01·European Journal of Clinical Microbiology & Infectious Diseases
Multiple regional outbreaks caused by global and local VIM-producing Klebsiella pneumoniae clones in Poland, 2006–2019
Article
作者: Palma, Federica ; Żabicka, Dorota ; Gniadkowski, Marek ; Izdebski, Radosław ; Biedrzycka, Marta ; Brisse, Sylvain ; Urbanowicz, Paweł
3
项与 RECK 相关的新闻(医药)2023-10-20
·生物谷
该研究以Wnt7a的合成、分泌和激活入手,阐释了脂修饰的Wnt蛋白是如何在ER中完成由PORCN向WLS的转移,WLS如何在细胞表面释放Wnt,以及中枢神经中Wnt7 特异性共受体RECK是如何发挥功
德克萨斯大学西南医学中心李晓淳实验室在 Cell 期刊发表了题为:Molecular basis of Wnt biogenesis, secretion and Wnt7 specific signaling 的研究论文【2】。
该研究以Wnt7a的合成、分泌和激活入手,阐释了脂修饰的Wnt蛋白是如何在ER中完成由PORCN向WLS的转移,WLS如何在细胞表面释放Wnt,以及中枢神经中Wnt7 特异性共受体RECK是如何发挥功能的。
为了鉴定ER中参与Wnt蛋白合成的因子, 研究团队在HEK293细胞中共表达了Wnt7a-WLS-RECK复合物。电镜结构显示出一个未知内源性蛋白结合Wnt7a,质谱鉴定和AlphaFold结构预测指出该蛋白为钙网蛋白(calreticulin,CALR)。CALR的Lectin 结构域主要作用于Wnt7a 的第295位天冬酰胺糖基化修饰,此修饰位点在大部分Wnt中保守。当在Wnt7a或Wnt3a中突变掉该糖基化位点时,突变体丧失了与CALR的结合能力,同时分泌量减少,激活下游信号能力显著减弱。
为了探究Wnt蛋白在被PORCN脂化时是否有CALR参与,研究团队共表达了PORCN和Wnt蛋白,CoIP实验显示,在Wnt蛋白存在的情况下,过表达的PORCN,内源WLS,内源CALR能够和Wnt蛋白形成四元复合物,加上对结构的分析,研究团队得出CALR通过稳定Wnt蛋白来帮助其从PORCN到WLS转运的结论。研究团队对其他18种Wnt蛋白进行氨基酸序列比对和CoIP实验,结果显示除了Wnt8a、Wnt8b、Wnt9a和Wnt9b,CALR参与其他15种Wnt的合成,揭示了CALR对于Wnt蛋白的折叠,转运和合成中具有重要作用。
为了进一步探究Wnt蛋白是如何从WLS上释放的,研究团队又解析了单独的WLS结构。与Wnt7a-WLS复合物结构对比发现,复合物的WLS跨膜区间结合了一个磷脂分子,该结果与已经报道的Wnt8a-WLS结构(Cell 184:194)和Wnt3a-WLS结构(Nature Communications 12: 4541)类似。但是单独的WLS并没有结合磷脂分子,而且其跨膜区发生了显著的构像变化,使结合Wnt蛋白hairpin2和脂修饰的口袋闭合。另外,虽然磷脂分子没有直接参与和Wnt7a的互作,但是CoIP实验和分子动力学实验证明磷脂分子对于WLS结合Wnt7a非常重要,因此该研究首次提出由磷脂分子介导的Wnt从WLS释放模型。有趣的是,通过分析单独的WLS结构,他们发现WLS跨膜区存在一个空腔,可以作为其抑制剂的结合位点,抑制Wnt的分泌,为靶向WLS的药物设计提供了重要依据。
此外,通过对Wnt7a-RECKCC4复合物结构的分析,作者发现作为Wnt7a的特异受体, RECK的CC4结构域结合在Wnt7a的N端结构域。参与RECK互作的氨基酸在其他17种Wnt蛋白里面是不保守的,突变二者相互作用的氨基酸会减弱Wnt7a介导的信号活性,从而揭示了RECK实现对Wnt7特异性的机理。
Wnt合成分泌以及Wnt7a信号通路示意图
总而言之,这项工作通过结构生物学,生物化学和细胞生物学的方法鉴定了第一个Wnt合成中的伴侣蛋白,提出了Wnt合成和分泌的新模型,并且阐释了Wnt7共受体的作用。该研究为抗癌药物研发,中枢神经中血脑屏障修复提供了分子模型。
临床结果临床1期
2023-06-29
·生物谷
本文中,小编整理了多篇重要研究成果,共同解读近年来科学家们在血脑屏障研究领域取得的新进展,分享给大家!
本文中,小编整理了多篇重要研究成果,共同解读近年来科学家们在血脑屏障研究领域取得的新进展,分享给大家!
【1】Sci Adv:科学家揭示一种跨越机体大脑血脑屏障的新型机制
doi:10.1126/sciadv.adg6618
血脑屏障是一种非常严格几乎无法穿透的细胞层,其能保护大脑不受血液中诸如毒素或细菌等因子的危害;血脑屏障只能允许非常有限的小分子通过,比如营养物质等,然而,这一保护层让科学家们难以研究大脑以及涉及能治疗大脑相关疾病的新型疗法。
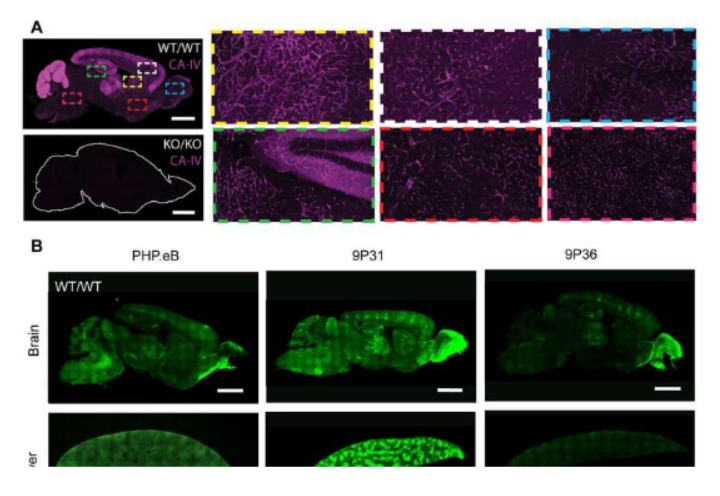
近日,一篇发表在国际杂志Science Advances上题为“Primate-conserved carbonic anhydrase IV and murine-restricted LY6C1 enable blood-brain barrier crossing by engineered viral vectors”的研究报告中,来自加州理工学院等机构的科学家们通过研究识别出了此前未知的一种机制,即特定的病毒载体(一种工程化改造携带多种所需货物的蛋白质外壳)穿越机体血脑屏障的机制,对这一机制的理解或能提供一种新方法来帮助设计用于研究和治疗用途的病毒载体,而理解这一机制及其它新型机制也能帮助解释大脑的防御机制是如何被新出现的病原体利用的,从而就能促使研究人员准备好阻断其发挥破坏作用的方法。
科学家揭示一种跨越机体大脑血脑屏障的新型机制。
图片来源:Science Advances (2023). DOI:10.1126/sciadv.adg6618
尽管血脑屏障能作为大脑强大的防御系统,但某些病毒已经自然进化出了能绕过它的能力。几十年来,研究人员一直在研究如何利用这类病毒作为一类穿越血脑屏障的特洛伊木马,为了实现这一点,研究人员筛选出了病毒所携带的原始病毒“货物”,随后利用其空壳来运送有益的治疗性药物或研究工具。拥有穿越血脑屏障能力的病毒载体能通过简单的血液注射将所需的基因运送到大脑中,因此并不需要在大脑中进行侵入性的注射,但不幸的是,大多数源于自然进化的病毒无法有效穿越机体的血脑屏障,因此其就必须高剂量给药,这无形中就会增加机体出现副作用的风险。
【2】Nat Commun:科学家有望利用新型WNT信号通路来恢复机体大脑血脑屏障的功能
doi:10.1038/s41467-023-37689-1
每个人心中都有一个保镖,即血脑屏障,其是血管和大脑其它部分之间的一层细胞,能将毒素、病原体和其它可能破坏大脑珍贵灰质组织的不良物质“踢”出去;当保镖失去警惕,一种不良的因素穿过血脑屏障后就会发生多种情况,侵入血脑屏障的癌细胞就能发展成为肿瘤组织,而当太多白细胞滑过血脑屏障,导致对大脑神经的保护层发生自身免疫攻击,从而阻碍其与机体其它部分相互交流时,就会引发多发性硬化症。
近日,一篇发表在国际杂志Nature Communications上题为“Therapeutic blood-brain barrier modulation and stroke treatment by a bioengineered FZD4-selective WNT surrogate in mice”的研究报告中,来自斯坦福大学医学院等机构的科学家们通过研究有望利用一种新型的WNT信号通路来恢复大脑的血脑屏障。研究者表示,血脑屏障的渗漏是多种脑补疾病发生的共同途径,因此,能够封堵住渗透的血脑屏障一直是医学界科学家们长期追寻的目标,目前修复血脑屏障的方法仍未得到充分的研究,这篇文章中,研究人员就描述了一种有望恢复这一屏障正常功能的新型疗法。
研究者Calvin Kuo说道,我们已经评估了一类新型治疗性分子用于治疗渗漏的血脑屏障,此前并没有专门针对血脑屏障的治疗性手段;文章中,研究人员通过研究WNT信号开始了他们的探索,WNT信号是细胞用来促进组织再生和伤口愈合的特殊交流通路,WNT信号能通过促进排列在血管中的细胞间的交流沟通从而维持血脑屏障的功能。有很多历史数据表明,WNT信号通路对于维持血脑屏障的功能非常重要,这样研究人员就能检测WNT信号通路,其能通过选择性地结合一种名为“卷曲受体”(frizzled receptor)的受体来开启血脑屏障中的特殊信号。
【3】Nat Commun:科学家成功追踪机体大脑血脑屏障的渗漏 或有望帮助开发治疗人类癫痫症的新型疗法
doi:10.1038/s41467-023-36070-6
在癫痫症研究中,长期以来科学家们一直认为,血脑屏障的渗漏是诱发大脑炎症的原因,近日,一篇发表在国际杂志Nature Communications上题为“Subcellular analysis of blood-brain barrier function by micro-impalement of vessels in acute brain slices”的研究报告中,来自波恩大学医院等机构的科学家们通过研究利用一种新方法证明了血液和中枢神经系统之间的屏障基本上能保持完好,他们所使用的方法有望为揭示癫痫症的发生提供新的线索,并能大大优化制药行业中的药物开发。
人类大脑中500公里的血管会排列成10平方米的薄细胞层,即血脑屏障(BBB,blood-brain barrier),其能保护大脑抵御有害物质和病原体的侵袭,同时其还能将大脑与机体其它器官联系起来;如果这一选择性屏障发生泄漏的话就会诱发诸如帕金森疾病、多发性硬化症和阿尔兹海默病等多种人类疾病,血脑屏障的功能异常对于大脑中肿瘤的发生也非常重要。
研究人员希望能阐明这些相互作用背后的真相,为了在细胞水平上研究血脑屏障的运输机制,研究人员在急性大脑切片上开发了基于微吸管的局部毛细血管灌注(毛细血管是机体最细的血管),并将其与与多光子显微镜进行结合。研究者Dirk Dietrich教授说道,我们将在研究中调查血脑屏障的新型分子技术比作一个干瘪的自行车轮胎,如果轮胎失去了空气,其并不会知道漏气的地方,这就是为何我们在补胎时会将充气的自行车内胎放置在水中来识别其漏气的地方的原因了,而这一原理也是研究者所采用的方法的基础,他们利用一种微吸管从内部向微血管注入液体,随后在多光子显微镜下来观察泄露的情况。
【4】Nature Communications: 血脑屏障调节的微血管稳定预防癫痫发作
doi: 10.1038/s41467-022-29657-y
癫痫影响全世界多达7000万人,其特点是反复无端癫痫发作。虽然有治疗癫痫的有效药物,但多达三分之一的药物对抗癫痫药无效。因此,迫切需要找到方法,将原本对药物有抵抗力的人转变为对药物有反应的人。虽然某些疾病,如德雷维特综合征,是癫痫的明确遗传原因,但在大多数情况下,癫痫的病因是未知的。然而,中风、脑瘤和创伤性脑损伤等情况会导致症状性癫痫发作活动的发展,并导致癫痫。
血脑屏障(BBB)功能障碍与癫痫预后恶化有关,但BBB功能障碍的潜在分子机制仍有待阐明。紧密连接蛋白是血脑屏障完整性的重要调节因子,尤其是紧密连接蛋白claudin-5在脑内皮细胞中含量最高,并调节血脑屏障的大小选择性。此外,claudin-5的表达中断与包括精神分裂症、抑郁症和创伤性脑损伤在内的许多疾病有关,但它在癫痫中的作用尚未完全破译。近日,都柏林三一学院研究者在Nature Communications杂志上发表了题为“Microvascular stabilization via blood-brain barrier regulation prevents seizure activity”的文章。在本研究中研究者认为稳定血脑屏障的药物可以代表新一代药物来预防癫痫患者的癫痫发作活动。
耐药性颞叶癫痫导致血脑屏障渗漏和海马区Cldn5表达下调。
图片来源: https://doi.org/10.1038/s41467-022-29657-y
在此,研究者报告了难治性癫痫患者手术切除的脑组织中claudin-5蛋白水平显著降低。与此同时,这些患者的动态增强MRI显示广泛的血脑屏障破坏。研究者发现,海马区claudin-5的靶向破坏或claudin-5的遗传杂合性会加剧红藻氨酸诱导的癫痫发作和血脑屏障的破坏。此外,在小鼠中,可诱导的Claudin-5基因敲除会导致自发的反复发作、严重的神经炎症和死亡。最后,研究者发现RepSox,一个claudin-5表达的调节者,可以预防实验性癫痫的发作活动。
【5】Nature:新研究构建人类血脑屏障的分子图谱
doi:10.1038/s41586-021-04369-3
近日,一篇发表在国际杂志Nature上题为“A human brain vascular atlas reveals diverse mediators of Alzheimer’s risk”的研究报告中,来自美国和德国多个研究机构的研究人员开发出一种方法来构建人类血脑屏障的分子图谱。在这篇论文中,他们描述了他们如何构建这种分子图谱,以及它所揭示的关于阿尔茨海默病等疾病的情况。
正如这些作者所指出的那样,这种血管系统在大多数脑部疾病中发挥着重要作用,然而人们对它的了解仍然不是很充分。他们认为其原因是缺乏人脑血管的分子图谱。他们指出,由于人死后很难从大脑中提取细胞和细胞核,所以这样的图谱还没有建立。这是因为它们往往会滞留在基底膜上。在这项新的研究中,他们找到了解决这个问题的方法,以构建在健康状态下和已死的患有阿尔茨海默病的人的大脑血管的分子图谱。
这项研究涉及寻找一种方法来对大脑血管系统的细胞核进行RNA分析。他们开始使用几种不同类型的化学物从基底膜中提取细胞。在多次不成功的尝试后,他们发现他们能够将一种曾用于分离脾细胞的方法改进为分离血管细胞,同时也能协助清理与大脑死亡有关的碎片。他们将他们的过程命名为血管分离和细胞核提取测序(vessel isolation and nuclei extraction for sequencing, VINE-seq)。他们的测试显示它在分离血管细胞方面非常有效。
【6】Neuron:揭示一种调节哺乳动物血脑屏障渗透性的新机制
doi:10.1016/j.neuron.2022.02.017
血脑屏障在保护中枢神经系统免受有害细菌、毒素和其他血源性病原体侵害方面发挥着重要作用。血脑屏障由一排紧密的内皮细胞组成,具有半渗透性和高度选择性。它允许小分子和营养物从血液进入中枢神经系统,同时阻止可能导致感染、炎症和其他破坏中枢神经系统微妙平衡的物质。然而,究竟是什么控制了血脑屏障的渗透性(即通透性),这是一个长期困扰着科学家们的问题。美国哈佛医学院布拉瓦特尼克研究所神经生物学教授Chenghua Gu博士研究了这个问题近十年。
此前,Gu和她的团队确定了一种称为转胞吞作用(transcytosis)的细胞运输系统通过决定分子在血脑屏障上运输的容易程度,在控制血脑屏障的渗透性方面起着关键作用。如今,在一项针对小鼠的新研究中,Gu团队揭示了关于这一过程如何受到调节的更多细节。他们描述了周围环境(即微环境)中的细胞向构成血脑屏障的细胞发出信号的一种机制。他们发现,这种细胞间的交流抑制了转胞吞作用,使血脑屏障的渗透性降低,确保分子不能轻易通过。相关研究结果于2022年3月15日在线发表在Neuron期刊上,论文标题为“Pericyte-to-endothelial cell signaling via vitronectin-integrin regulates blood-CNS barrier”。
Gu说,“我们的研究为更好地理解微环境如何维持血脑屏障以及为何对维持血脑屏障很重要打开了大门,这可以为开发更好的实验室模型来研究血脑屏障提供参考。”这些作者说,不仅如此,该机制还提供了一种操纵血脑屏障的潜在途径,使其更容易或更难渗透。如果这些发现在进一步的动物研究中得到重现,然后在人类身上得到重现,它们可能会指出治疗疾病或向大脑递送药物的新方法。
【7】Science:揭示一类新的分子可修复神经障碍中的血脑屏障缺陷
doi:10.1126/science.abm4459
许多令人印象深刻的大脑病变与主要的脑血管缺陷密切相关,而目前由于缺乏药物,这些缺陷无法得到治疗。近日,一篇发表在国际杂志Science上题为“Engineered Wnt ligands enable blood-brain barrier repair in neurological disorders”的研究报告中,来自比利时布鲁塞尔自由大学的研究人员取得特别有希望的发现:他们不仅开发出一类新的特异性校正这些功能障碍的分子:工程化的Wnt,而且还在完全不同的大脑病变的小鼠模型中展示了它们的有效性。
Wnt7a配体在血脑屏障缺陷治疗中的应用。
图片来源:Science, 2022, doi:10.1126/science.abm4459。
Vanhollebek团队专门研究脑血管及其功能障碍。通过研究在胚胎期控制这些血管形成的蛋白,他们认为他们可以确定具有良好治疗潜力的靶标:Gpr124/Reck膜复合物,它的作用之前已在神经发育背景下揭示出。他们发现的证据是通过开发靶向Gpr124/Reck膜复合物的分子,他们成功地减缓了小鼠胶质母细胞瘤(最常见的成年原发性脑癌)的进展,并减少了中风后的病变。
Vanhollebek团队此前在Science期刊上发表了关于这种治疗靶标的机制特征。这项新研究确定了它在小鼠身上的治疗潜力。当该靶标遭受激活时,因病变而变得过度具有渗透性的功能失调的脑血管恢复了其原有的功能;它们恢复了一系列强烈限制血液和神经组织之间交流并被统称为血脑屏障(blood-brain barrier)的细胞和分子特征。因此,大脑再次受到保护,不受血液中循环的有毒成分的影响,而且大脑病变的进展也减缓了。
【8】Sci Adv:科学家开发出新型DNA纳米管 或能运输治疗性制剂跨越血脑屏障靶向作用胶质母细胞瘤
doi:10.1126/sciadv.abl5872
胶质母细胞瘤被广泛认为是一种最具侵袭性的脑癌,即使患者经过治疗,其存活率也相当低,大部分患者在诊断后平均只能存活15-18个月,由于胶质母细胞瘤的肿瘤会表现出高度多样化的特征以及其在体内所处的位置(处于敏感和受保护的大脑区域),因此治疗这种疾病对于科学家们而言极具挑战性。近日,一篇发表在国际杂志Science Advances上题为“ssDNA nanotubes for selective targeting of glioblastoma and delivery of doxorubicin for enhanced survival”的研究报告中,来自约翰霍普金斯大学等机构的科学家们通过研究开发了一种新型的基于DNA纳米技术的药物运输系统,其或能通过靶向作用原发性肿瘤来改善患者的疗法和其生存率。
研究者Efie Kokkoli教授说道,通过血液运输疗法最大的障碍之一就是如何穿过血脑屏障,血脑屏障不仅能保护大脑免于血液中的有毒物质,还能阻挡诸如治疗性药物等大分子物质;为此我们利用DNA纳米技术开发出了一种单链DNA(ssDNA)纳米管,其就能跨越血脑屏障,并靶向作用大脑中的肿瘤。DNA纳米技术能帮助研究人员利用合成性的DNA进行多种技术目的;这篇研究中,研究人员利用ssDNA和其它分子设计出了一种能携带治疗制剂的自组装纳米管,这种合成性的DNA就能帮助研究人员设计出靶向作用特定细胞的新型策略。
因此,纳米管不仅是一个包裹,其还是一种信使,能将药物运输到靶向位点;文章中,研究者Kokkoli及其同事利用小鼠模型检测了ssDNA纳米管在靶向作用胶质母细胞瘤上的准确定,他们将纳米管插入到小鼠大脑半球的两侧,一侧是健康的,另一侧则生长有胶质母细胞瘤;研究者观察到,肿瘤会紧紧抓住纳米管,但健康一侧的大脑中则没有这种纳米管,这就证实了这种新方法或许损伤健康细胞的可能性不大。随后研究人员将纳米管插入到小鼠尾部的静脉中,结果观察到了相同的结果,这就表明,这种新型纳米管能成功穿过啮齿动物大脑中的血脑屏障。
【9】Science子刊:临床试验表明聚焦超声可以递送抗体药物通过血脑屏障来治疗乳腺癌脑转移
doi:10.1126/scitranslmed.abj4011
近日,一篇发表在国际杂志Science Translational Medicine上题为“MR-guided focused ultrasound enhances delivery of trastuzumab to Her2-positive brain metastases”的研究报告中,来自加拿大多伦多辛尼布鲁克健康科学中心的研究人员证实,磁共振引导下的聚焦超声可用于安全地将抗体药物递送到已转移到大脑中的乳腺癌。在这项针对Her2阳性乳腺癌患者的I期临床试验中,这些作者在使用Insightec公司的Exablate Neuro聚焦超声设备暂时无创地打开血脑屏障(BBB),使静脉注射的曲妥珠单抗(trastuzumab,也称为赫赛汀)更有效地进入肿瘤部位后,捕捉到了抗体疗法曲妥珠单抗的图像。
MR图像显示通过血脑屏障聚焦超声递送抗体治疗后转移性肿瘤的大小缩小。
图片来源:Sunnybrook Health Sciences Centre。
抗体药物可以帮助免疫系统对抗癌细胞,而且它们经常与放疗和化疗结合使用。然而,当试图靶向大脑中的部位时,血脑屏障是一个挑战。血脑屏障是血管内壁的一层细胞,保护大脑不受病毒、细菌和其他毒素的侵害,但它也能阻止诸如曲妥珠单抗之类的治疗性药物以足够高的浓度到达大脑,从而发挥疗效。研究者Nir Lipsman博士说,“这是首次直观地证实聚焦超声可以改善靶向抗体药物穿过血脑屏障。这些研究结果是初步的但非常有希望的,随着研究的继续,其影响远远超出了脑癌,它们也对血脑屏障对药物递送带来挑战的其他神经系统疾病(包括帕金森病和阿尔茨海默病)产生了影响。”
在这项临床试验中,共有10名患者参与其中,但是这些作者目前仅公布了其中的4人的初步结果。转移性乳腺癌,也被称为第四阶段乳腺癌,开始于乳房,可以扩散到大脑、骨骼、肝脏或其他器官。目前对乳腺癌脑转移的治疗包括开放性神经外科手术、放疗和化疗。然而,根据脑转移的位置和数量,手术和放疗的选择可能是有限的,而且治疗方法可能很难有效地到达大脑中的肿瘤。
【10】Nature:揭示Ω-3脂肪酸跨越血脑屏障进行运输的结构基础
doi:10.1038/s41586-021-03650-9
二十二碳六烯酸(docosahexaenoic acid)是一种对神经系统发育和功能非常重要的Ω-3脂肪酸,其主要是通过饮食来源从而供给给大脑和眼睛,这种营养物质能以溶血卵磷脂的形式被运输通过血脑屏障和血液视网膜屏障,整个运输过程则是被主要促进超家族结构域2A(MFSD2A)以一种Na+依赖性的方式来完成的。近日,一篇发表在国际杂志Nature上题为“Structural basis of omega-3 fatty acid transport across the blood–brain barrier”的研究报告中,来自哥伦比亚大学等机构的科学家们通过研究发现,Ω-3脂肪酸有望作为打开机体血脑屏障的关键。
研究者表示,一种将Ω-3脂肪酸运送到大脑中的分子壮观图像或能提供一种策略来将神经性疗法运送到大脑中。文章中,研究人员设法获得了为Ω-3脂肪酸进入大脑提供通道的转运蛋白的三位结构,在这一结构中,研究人员揭示了Ω-3脂肪酸与转运蛋白相互结合的机制,相关信息或能帮助设计出新型药物,来模拟Ω-3脂肪酸从而拦截这一系统并进入大脑。
治疗神经性疾病所面临的主要挑战就是如何让药物穿过血脑屏障,血脑屏障是一层由密密麻麻的细胞排列分布在大脑血管中的结构,其能帮助阻断毒素、病原体和某些营养物质进入大脑中,很不幸的是,血脑屏障还能阻断很多原本寄希望于能治疗神经系统疾病的药物进入大脑。诸如Ω-3脂肪酸等必要的营养物质需要专门的转运蛋白,这些转运蛋白能特异性地识别Ω-3脂肪酸并促进其穿过血脑屏障。让Ω-3脂肪酸进入的转运蛋白名为MFSD2A,同时其也是研究人员研究的重点,理解MFSD2A的特性以及其如何让Ω-3脂肪酸穿过血脑屏障或能为研究人员提供关键信息,来帮助设计出治疗疾病的新型药物。(生物谷Bioon.com)
生物谷更多精彩盘点!敬请期待!
抗体药物偶联物
2022-12-12
·生物谷
该论文基于齐碳纳米孔基因测序平台,对临床新出现的携带tmexCD-toprJ的肺炎克雷伯菌进行了广泛研究,是对其流行病学研究的有效补充。
细菌耐药性问题已成为一个世界性的难题。质粒等可移动元件介导的耐药基因水平传播所致革兰阴性菌耐药性的快速出现和散播,引起了全球高度关注。
外排泵(efflux pumps)是细菌将胞内的药物或毒性物质排出胞外的蛋白转运系统,也是临床上细菌对抗菌药物耐药的主要机制之一。近年来,携带可移动的多重耐药外排泵基因簇(tmexCD-toprJ)的肺炎克雷伯菌在我国临床患者、动物和零售肉类样本中不断发现,其介导了对包括替加环素这一人类面临多重耐药肠杆菌科细菌感染的“最后一道防线”在内的多重耐药性。
近日,北京大学第三医院沈宁教授团队、清华大学附属北京清华长庚医院郭军教授团队联合齐碳科技,在微生物学顶级期刊期刊 The Lancet Microbe 上在发表了题为:Dissemination of the mobilised RND efflux pump gene cluster tmexCD-toprJ among Klebsiella pneumoniae 的研究论文【1】。
该论文基于齐碳纳米孔基因测序平台,对临床新出现的携带tmexCD-toprJ的肺炎克雷伯菌进行了广泛研究,是对其流行病学研究的有效补充。
2022年10月,浙江大学医学院附属第二医院张嵘教授等通过在我国的临床监测研究和对公共数据的深度挖掘,首次发现编码可移动RND型多耐药外排泵的tmexCD-toprJ基因簇已经在多种临床重要致病菌中播散【2】,包括假单胞菌属、克雷伯菌属、气单胞菌属和变形杆菌属等。并在研究中发现发现多种肺炎克雷伯菌序列型(ST)携带tmexCD-toprJ基因簇,包括ST1、ST11、ST147、ST15、ST2667、ST273、ST2909、ST3447、ST490和ST571。
此次北医三院、清华长庚医院团队基于齐碳纳米孔基因测序平台的研究,历经2017年1月至2022年4月的长期监测,从1484株临床分离的肺炎克雷伯菌中首次发现了上述10种ST型外的3种携带tmexCD1-toprJ1的全新ST型菌株,总体阳性率为0.88%(13/1484),包括1个同时携带编码碳青霉烯酶的blaKPC-2和blaNDM-1基因的泛耐药ST22克隆(11株菌株)、1株多耐药ST3691菌株和1株多耐药ST37菌株。这些菌株菌均呈现替加环素耐药,最低抑菌浓度为4-24mg/L。
同时,研究团队还发现1株替加环素敏感的ST11型菌株携带了5'端发生缺失的tmexD1基因和toprJ基因,而tmexC1基因完全缺失。这表明只有完整的tmexCD1-toprJ1基因簇才能介导替加环素耐药,与张嵘教授等在其研究中发现通过敲低tmexD基因表达可降低菌株替加环素耐药性的结果一致。
此外,这株ST11型菌株与其他研究已发表的两株分离自中国养鸡场苍蝇样本的菌株、三株猪源菌株和其他三株人源菌株聚集在一个分支中;这株菌中,编码5'端缺失tmexD1基因和完整toprJ基因的质粒与1株分离自零售猪肉的ST147型菌株中的编码完整tmexCD1-toprJ1基因簇的质粒高度相似。克隆群258(CC258)主要由ST258和ST11型构成,其中ST11型在我国临床、社区和畜牧业中均为主要流行的肺炎克雷伯菌亚型,而携带tmexCD1-toprJ1的ST11型菌株在屠宰场中也有发现。
这些结果表明,临床中发现的携带tmexCD1-toprJ1肺炎克雷伯菌可能与养殖动物及相关环境中的耐药菌株具有密切关联。
该研究中发现的携带tmexCD1-toprJ1基因簇的ST型。(A)已发现的携带tmexCD1-toprJ1基因簇的肺炎克雷伯菌ST型的最小生成树,其中红色圆圈代表本研究中发现的ST型,蓝色圆圈代表在此前研究中已发现的其他ST型。(B)本研究中发现的3种ST型中tmexCD1-toprJ1基因簇、1株ST11菌株中5‘端发生缺失的tmexD1基因和完整toprJ基因所在的基因环境。其中红色箭头代表耐药基因,蓝色箭头代表整合酶、重组酶和转座酶基因,灰色箭头代表其他功能基因。(C)携带5‘端缺失tmexD1基因的ST11菌株与已发表基因组序列的ST11菌株的系统发生树。本研究从GenBank数据库中收集了1675株ST11型菌株的基因组序列共同进行分析,本图中展示了和本研究获得的ST11菌株PEKP3038聚集在同一分支的45个基因组。蓝色框中包含了PEKP3038和另外三株携带tmexCD1-toprJ1基因簇的猪源菌株(红色字体)。
该研究基于齐碳QNome测序平台的长读长优势,为临床多重耐药研究提供更多理论依据。以上研究发现是对携带tmexCD1-toprJ1肺炎克雷伯菌流行病学的有效补充,表明tmexCD1-toprJ1基因簇可能在肺炎克雷伯菌中已经发生了广泛播散。
因此,急需在“One Health“理念下,在医疗机构、社区及肉用动物养殖和加工业中加强相应的流行病学监测,以控制携带TMexCD1-TOprJ1外排泵菌株的进一步传播。
随着齐碳科技纳米孔测序技术的进步与不断升级优化,我们也期待其在医疗健康、食品安全、动植物疫病防控、环境监测保护、司法鉴定等更广泛的场景中的应用。
临床研究微生物疗法
分析
对领域进行一次全面的分析。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用