预约演示
更新于:2026-02-14
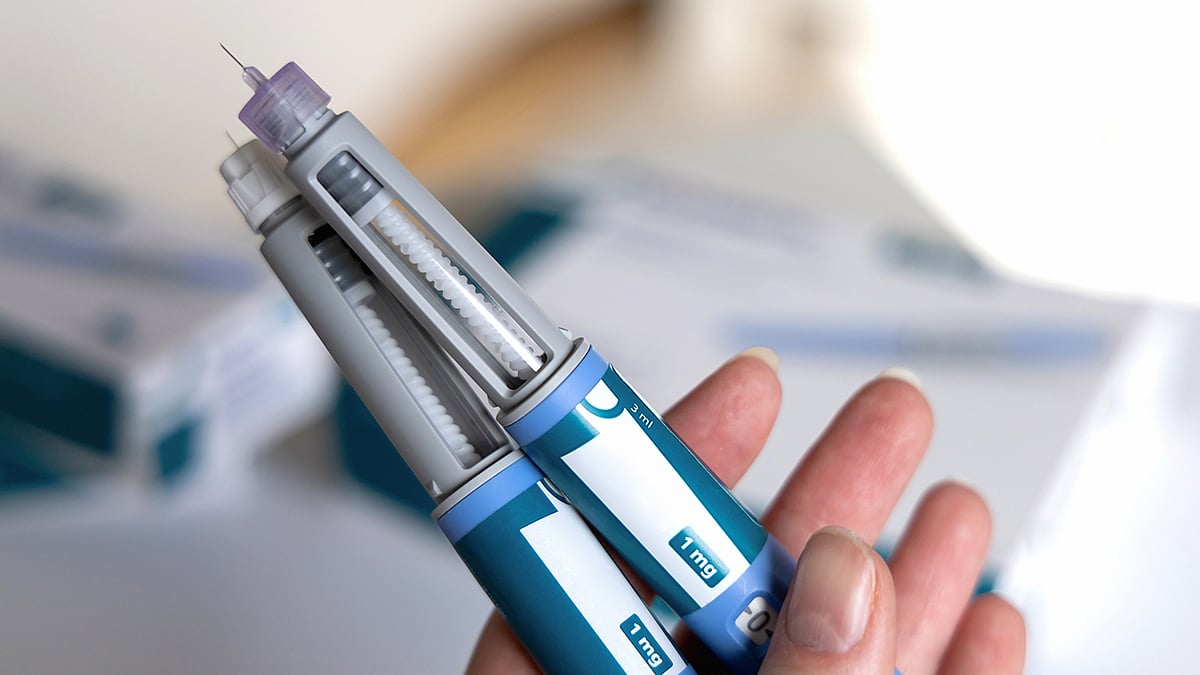
Semaglutide (Thery Pharmaceutical)
司美格鲁肽(特瑞药业)
更新于:2026-02-14
概要
基本信息
原研机构 |
在研机构 |
非在研机构- |
权益机构- |
最高研发阶段临床3期 |
首次获批日期- |
最高研发阶段(中国)临床3期 |
特殊审评- |
登录后查看时间轴
关联
3
项与 司美格鲁肽(特瑞药业) 相关的临床试验CTR20244777
司美格鲁肽注射液治疗中国肥胖人群的多中心、随机、开放、平行、阳性药物对照的 Ⅲ 期临床研究
主要目的:比较司美格鲁肽注射液与原研药物在中国肥胖人群中减重的有效性。次要目的:比较司美格鲁肽注射液与原研药物的安全性,比较司美格鲁肽注射液与原研药物的免疫原性。
开始日期2025-03-26 |
申办/合作机构 |
CTR20243970
司美格鲁肽注射液在健康成人受试者中的药代动力学特征比较的随机、开放、平行入组的I期临床研究
比较单次皮下注射试验药物司美格鲁肽注射液(规格:1.5mL:1mg)与对照药物司美格鲁肽注射液(商品名:Wegovy®,规格:1.5mL:1mg)后在中国健康成人受试者体内的药代动力学特征和安全性。
开始日期2024-10-30 |
申办/合作机构 |
CTR20241707
司美格鲁肽注射液在健康成人受试者中的药代动力学特征比较的随机、开放、平行入组的I期临床研究
比较皮下注射试验药物司美格鲁肽注射液与对照药物司美格鲁肽注射液后在中国健康成人受试者体内的药代动力学特征和安全性
开始日期- |
申办/合作机构 |
100 项与 司美格鲁肽(特瑞药业) 相关的临床结果
登录后查看更多信息
100 项与 司美格鲁肽(特瑞药业) 相关的转化医学
登录后查看更多信息
100 项与 司美格鲁肽(特瑞药业) 相关的专利(医药)
登录后查看更多信息
74
项与 司美格鲁肽(特瑞药业) 相关的文献(医药)2026-01-01·Med
Semaglutide for the treatment of cognitive dysfunction in major depressive disorder: A randomized clinical trial
Article
作者: McIntyre, Roger S ; Shah, Hiya ; Di Vincenzo, Joshua D ; Badulescu, Sebastian ; Armanyous, Michael ; Llach, Cristian-Daniel ; Mansur, Rodrigo B ; Brudner, Ryan ; Gill, Hartej ; Rosenblat, Joshua D ; Tabassum, Aniqa ; Phan, Lee
BACKGROUND:
Evidence suggests that glucagon-like peptide 1 receptor agonists (GLP-1RAs) might have pro-cognitive effects. No prior study has evaluated the efficacy and safety of a GLP-1RA for the treatment of cognitive dysfunction in adults with major depressive disorder (MDD) in a randomized clinical trial.
METHODS:
This was a 16-week, randomized, double-blind, placebo-controlled, parallel-group trial (NCT04466345). Eligible adults met DSM-5-defined criteria for MDD, exhibited pre-treatment evidence of cognitive impairment, and were overweight/obese. Patients were randomized (1:1) to receive an adjunctive placebo or 14 mg oral semaglutide. The primary outcome was an executive function composite score comprising the digit symbol substitution test, the Stroop test, and the n-back test. Secondary outcomes included a global cognition composite score, measures of functioning, depressive symptom severity, suicidality, and body weight.
FINDINGS:
72 participants were randomized to oral semaglutide (n = 35) or placebo (n = 37). Semaglutide did not improve executive function (adjusted Z score difference [semaglutide - placebo]: 0.32, 95% confidence interval [CI]: -0.92 to 1.58, p = 0.60). Preplanned secondary analysis showed treatment effects for global cognition (2.39, 95% CI: 0.19 to 4.60, p = 0.03) and body weight (kg) (adjusted mean difference -6.03, 95% CI: -8.76 to -3.29, p < 0.001). Treatment did not affect depressive symptom severity or the frequency of suicidal ideation. Gastrointestinal side effects were common in the semaglutide group, with no serious adverse events.
CONCLUSION:
Semaglutide did not improve executive function; results from secondary analyses suggested effects on specific domains of cognition. Semaglutide was safe for patients with MDD.
FUNDING:
This work was supported by the Physicians' Services Incorporated Foundation.
2026-01-01·Asia-Pacific Journal of Ophthalmology
Does semaglutide increase the risk of non-arteritic anterior ischemic optic neuropathy? A systematic review and meta-analysis of emerging evidence
Review
作者: Chen, Kai-Yang ; Chan, Chi-Ming ; Chan, Hoi-Chun
BACKGROUND:
Semaglutide, a GLP-1 receptor agonist widely prescribed for type 2 diabetes and obesity, has recently been linked to rare ocular adverse events, including non-arteritic anterior ischemic optic neuropathy (NAION). Given the growing concerns and limited clarity, this systematic review and meta-analysis aims to critically assess the potential association between semaglutide use and NAION risk.
OBJECTIVES:
To evaluate the association between semaglutide use and the development of NAION.
METHODS:
A comprehensive literature search was conducted via different databases from inception to June 3rd, 2025. A reviewer screened the potential articles against prespecified eligibility criteria. The risk of bias in the eligible studies was then evaluated using the Newcastle Ottawa Scale (NOS). Data were then systematically extracted and analyzed.
RESULTS:
The database search yielded 3539 records, of which 10 research articles investigating the association between Semaglutide and NAION were included in this study. Semaglutide use was associated with a significantly increased risk of NAION compared to control medications, with a pooled hazard ratio of 2.620 (95 % CI: 1.808-3.795, P < 0.001). Risk elevation showed time-dependency, becoming statistically significant after 2 years of exposure. Identified risk factors included older age, male sex, prolonged diabetes duration, elevated HbA1c, diabetic retinopathy, and obesity. Among GLP-1 receptor agonists, semaglutide accounted for 86.5 % of reported NAION cases. Clinical presentations featured optic disc edema, intraretinal fluid on OCT, and crowded optic discs. Cumulative incidence rates were substantially higher in semaglutide users versus non-GLP-1 receptor agonist comparators.
CONCLUSIONS:
Semaglutide use shows association with increased NAION risk, particularly with prolonged exposure and in patients with predisposing factors. Risk-benefit assessment and targeted ophthalmologic monitoring are recommended while maintaining appropriate therapeutic use.
2026-01-01·Alzheimers & Dementia-Translational Research & Clinical Interventions
Baseline characteristics from evoke and evoke+: Two phase 3 randomized placebo‐controlled trials of semaglutide in participants with early‐stage symptomatic Alzheimer's disease
Article
作者: Scheltens, Philip ; Jeppesen, Rose ; Johannsen, Peter ; Bardtrum, Lars ; Hansen, Charlotte T ; Sano, Mary ; Atri, Alireza ; Zetterberg, Henrik ; Cummings, Jeffrey L ; Feldman, Howard H ; Colombo, Teresa León
Abstract:
INTRODUCTION:
The glucagon‐like peptide‐1 receptor agonist semaglutide may impact neuroinflammation and reduce neurodegeneration. We present baseline characteristics of participants enrolled in the evoke (NCT04777396) and evoke+ (NCT04777409) trials, referred to as “evoke (+)” hereafter.
METHODS:
Evoke (+) are two ongoing global, multicenter, randomized, double‐blind, parallel‐group, placebo‐controlled phase 3 trials investigating semaglutide in participants with early‐stage symptomatic Alzheimer's disease (AD) with confirmed amyloid positivity (by positron emission tomography or cerebrospinal fluid testing). Inclusion criteria are the same for both trials, except that by design, evoke+ also includes participants with significant small vessel pathology. Both trials include a 12‐week screening phase before randomization (1:1) to receive oral semaglutide titrated to 14 mg or placebo for 156 weeks. Baseline data were summarized and analyzed descriptively. Additionally, data were pooled and assessed by five main geographical regions.
RESULTS:
Evoke (+) recruited 9996 participants from 566 sites in 40 countries. The mean (standard deviation) age of participants was 71.8 (7.1) and 72.6 (7.1) years in evoke and evoke+, respectively; more participants were female than male (female: 53.0% and 51.9%, respectively) and most had a Clinical Dementia Rating (CDR) global score of 0.5 (72.8% and 71.4%; CDR global score of 1: 26.5% and 27.6%). Both trial populations had similar demographics, and clinical and cognitive baseline characteristics, except that 2.8% of participants in evoke+ had magnetic resonance imaging‐documented significant small vessel pathology as per protocol inclusion criteria. Regional‐level data demonstrated some differences in AD treatment characteristics, including cholinesterase inhibitor use of 41.7% in North America versus 61.6% in Asia.
DISCUSSION:
Evoke (+) are the only large‐scale, phase 3 trials investigating the longer‐term efficacy and safety of semaglutide in early AD as a potential disease‐modifying treatment. The baseline characteristics from evoke (+) reflect a varied, global population with early‐stage symptomatic AD. Primary readouts are expected in the second half of 2025.
Highlights:
evoke and evoke+ are the only large‐scale randomized controlled trials (RCTs) investigating the longer‐term efficacy and safety of semaglutide in early AD.Baseline characteristics reflect a varied, global population.The trials’ primary readouts are expected in the second half of 2025.
41
项与 司美格鲁肽(特瑞药业) 相关的新闻(医药)2026-01-07
WEDNESDAY, Jan. 7, 2026 — Ozempic and Wegovy might help people avoid colon cancer as well as promote weight loss or control diabetes, a new study says.
People who took a GLP-1 drug were 36% less likely to get colon cancer than people who took aspirin, according to findings scheduled for presentation Saturday at a meeting of the American Society of Clinical Oncology in San Francisco.
“While aspirin has been studied for colorectal cancer prevention, its modest benefit and bleeding risks limit its use,” said lead researcher Dr. Colton Jones , a hematology and oncology fellow at the University of Texas-San Antonio.
“GLP-1 receptor agonists, now widely prescribed for diabetes and obesity, may offer a safer option for both metabolic control and cancer prevention,” Jones said in a news release.
It’s estimated that 150,000 American were diagnosed with colon cancer in 2025 and more than 50,000 died of the disease, researchers said in background notes.
Glucagon-like peptide-1 (GLP-1) drugs mimic the GLP-1 hormone, which helps control insulin and blood sugar levels, decreases appetite and slows digestion of food. The best-known GLP-1 drugs are semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound).
For the new study, researchers analyzed health records for more than 281,000 people drawn from a commercial health care database.
Half were taking a GLP-1, and the other half aspirin. Researchers followed the GLP-1 group for about six years, and the aspirin group for about five years.
Results showed a 36% lower risk of colon cancer among those taking a GLP-1 drug.
Benefits were even greater — a nearly 42% lower risk — among people whose family or personal history put them at higher risk of colon cancer, researchers said.
Those taking GLP-1 drugs also were less likely to suffer side effects like kidney damage, stomach ulcers or GI bleeding than those on aspirin, researchers said.
However, diarrhea and abdominal pain were more common among those taking GLP-1 drugs.
Researchers warned that the overall benefit for any one person was small. Statistics showed that more than 2,000 people would need to take a GLP-1 drug for one person to have a lower risk of colon cancer.
However, an estimated 6% of Americans are taking GLP-1 drugs, researchers said. That could mean as many as 20 million Americans already are using GLP-1s, and subsequently benefiting from lower colon cancer risk.
As a whole, GLP-1s reduced risk of colon cancer, but when studied individually only semaglutide, liraglutide and dulaglutide had a significant effect, researchers said. Tirzepatide did not show the same significance.
The research team next plans to validate its findings in clinical trials.
“GLP-1 receptor agonists may have benefits far beyond the waistline,” said Dr. Joel Saltzman , vice chair of regional oncology at Taussig Cancer Center, Cleveland Clinic, who reviewed the findings.
“These findings show that they may be an important part of cancer prevention treatment strategies as well,” he continued in a news release. "The preventive benefits of aspirin, nonsteroidal anti-inflammatory drugs and statins in the development of colorectal cancer have been investigated for years. This real-world study suggests that the GLP-1 receptor agonists may have an exciting role in this area.”
Salzman said further research is a priority to understand the promise of these drugs to help prevent cancer.
Findings presented at medical meetings should be considered preliminary until published in a peer-reviewed journal.
Sources
American Society of Clinical Oncology, news release, Jan. 5, 2026
临床结果ASCO会议
2026-01-02
Adalvo will submit its DCP application for Semaglutide on February 13th, 2026, marking a major step forward in expanding access to high-value diabetes treatments.
Semaglutide, a GLP-1 receptor agonist, is recognized as one of the most transformational therapies of recent years, with proven efficacy in improving glycemic control and supporting weight management in adults with type 2 diabetes mellitus.
Adalvo’s DCP submission aligns with IP protection expiring globally in 2026. Backed by a clearly defined regulatory pathway, it positions the company for Day-1 launches in key markets.
Globally, Semaglutide sales were estimated to reach $33-$36Bn in 2024, with three-year CAGR exceeding 42%, underlining rapid market adoption.
Given the strong global demand for GLP-1 therapies, the company has implemented a robust double-sourcing strategy for the active pharmaceutical ingredient (API), drug manufacture, and delivery pen production.
Semaglutide is Adalvo's seventh peptide and confirms the company's position as holder of the broadest GLP-1 pipeline in B2B Pharma. The portfolio includes small molecules, oral and injectable formulations, and both short- and long-acting treatment options.
To discuss licensing or partnership opportunities within Adalvo’s diabetes portfolio, contact the team today.
2026-01-02
FRIDAY, Jan. 2, 2026 -- For patients at high cardiovascular risk with overweight or obesity, semaglutide is associated with reduced burden of total hospital admissions, according to a study published online Dec. 23 in JAMA Cardiology .
Stephen J. Nicholls, M.D., from Monash Victorian Heart Institute and Monash University in Australia, and colleagues conducted a prespecified exploratory analysis of the Semaglutide Effects on Cardiovascular Outcomes in People With Overweight or Obesity (SELECT) clinical trial to examine the impact of semaglutide on total hospital admissions and duration of hospital stay in patients aged 45 years or older with established cardiovascular disease (CVD) and body mass index of 27 kg/m 2 or higher without diabetes. In the SELECT trial, patients were randomized from October 2018 to March 2021 to subcutaneous semaglutide, 2.4 mg, or placebo once weekly. A total of 17,604 patients at 804 clinical settings were followed up for a median of 41.8 months.
The researchers found that there were 11,287 hospital admissions. Compared with placebo, semaglutide was associated with a lower number of total hospitalizations for any indication (18.3 versus 20.4 admissions per 100 patient-years; mean ratio, 0.90) and for serious adverse events (15.2 versus 17.1 admissions per 100 patient-years; mean ratio, 0.89). The semaglutide group also had a lower number of days hospitalized for any indication (157.2 versus 176.2 per 100 patient-years; rate ratio, 0.89) and for serious adverse events (137.6 versus 153.9 days per 100 patient-years; rate ratio, 0.89). In selected subgroups including body mass index, age, and sex, no heterogeneity was seen for the reduction of hospital admissions with semaglutide.
"These findings extend the previously reported benefits of semaglutide on major adverse cardiovascular events to a broader range of clinical and health care system outcomes," the authors write.
Several authors disclosed ties to the biopharmaceutical industry, including Novo Nordisk, which manufactures semaglutide and funded the study.
Abstract/Full Text (subscription or payment may be required)

AHA会议临床研究临床结果
100 项与 司美格鲁肽(特瑞药业) 相关的药物交易
登录后查看更多信息
外链
| KEGG | Wiki | ATC | Drug Bank |
|---|---|---|---|
| - | - | - |
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 肥胖 | 临床3期 | 中国 | 2025-03-26 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
No Data | |||||||
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或

药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或

临床分析
紧跟全球注册中心的最新临床试验。
登录
或

批准
利用最新的监管批准信息加速您的研究。
登录
或

生物类似药
生物类似药在不同国家/地区的竞争态势。请注意临床1/2期并入临床2期,临床2/3期并入临床3期
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
