预约演示
更新于:2026-01-29

The Cooper Health System, Inc.
更新于:2026-01-29
概览
标签
消化系统疾病
肿瘤
蛋白水解靶向嵌合体(PROTAC)
疾病领域得分
一眼洞穿机构专注的疾病领域
暂无数据
技术平台
公司药物应用最多的技术
暂无数据
靶点
公司最常开发的靶点
暂无数据
| 疾病领域 | 数量 |
|---|---|
| 肿瘤 | 1 |
| 排名前五的药物类型 | 数量 |
|---|---|
| 蛋白水解靶向嵌合体(PROTAC) | 1 |
| 排名前五的靶点 | 数量 |
|---|---|
| CDK9(细胞周期蛋白依赖性激酶9) | 1 |
关联
1
项与 The Cooper Health System, Inc. 相关的药物靶点 |
作用机制 CDK9 降解剂 |
在研适应症 |
非在研适应症- |
最高研发阶段临床前 |
首次获批国家/地区- |
首次获批日期- |
87
项与 The Cooper Health System, Inc. 相关的临床试验NCT07361549
Localized Injection of Lidocaine Via the Middle Meningeal Artery for Intractable Headache Treatment: A Randomized, Double-Blinded, Parallel Phase 2 Clinical Trial
The goal of this clinical trial is to test whether injecting lidocaine into two blood vessels of the brain can help treat chronic headaches (migraines)
开始日期2026-03-01 |
NCT07296120
Seroconversion Following RSV Vaccination in Bone Marrow Transplant and CAR-T Patients
This study evaluates whether the RSV vaccine Abrysvo can produce an antibody response in patients with blood cancers who have previously received a hematopoietic stem cell transplant (HSCT) or CAR-T cell therapy. The vaccine targets the prefusion F (preF) protein of RSV, which is an important component of protective immunity against the virus.
The main goal of the study is to measure the change in antibody levels against the preF protein four weeks after vaccination compared with levels before vaccination. The study will also assess whether participants develop a meaningful immune response, defined as at least a four-fold increase in RSV neutralizing antibody levels four weeks after vaccination.
The main goal of the study is to measure the change in antibody levels against the preF protein four weeks after vaccination compared with levels before vaccination. The study will also assess whether participants develop a meaningful immune response, defined as at least a four-fold increase in RSV neutralizing antibody levels four weeks after vaccination.
开始日期2026-01-01 |
申办/合作机构 |
NCT07042048
Placing External Ventricular Drains Using Assistive Augmented Reality or Image-Based Localization: A Randomized Controlled Clinical Trial (PEARL)
The goal of this clinical trial is to assess if EVD placement using augmented reality is non inferior to image-guidance systems for assistance in adult patients needing an EVD for spontaneous ICH with IVH or severe TBI. The main question it aims to answer is:
Can EVDs be placed successfully with at least equal safety and efficacy using augmented reality devices in comparison to using standard image-guidance techniques?
Can EVDs be placed successfully with at least equal safety and efficacy using augmented reality devices in comparison to using standard image-guidance techniques?
开始日期2025-07-01 |
100 项与 The Cooper Health System, Inc. 相关的临床结果
登录后查看更多信息
0 项与 The Cooper Health System, Inc. 相关的专利(医药)
登录后查看更多信息
1,212
项与 The Cooper Health System, Inc. 相关的文献(医药)2026-02-01·JOURNAL OF CRITICAL CARE
Authors' response: “Observational study of cefepime therapeutic drug monitoring in continuous venovenous hemodialysis”
Letter
作者: Hanretty, Alexandra ; Delic, Justin ; Wageh, John ; Kim, Soyoung ; Pasciolla, Stacy ; Igneri, Lauren A ; Kludjian, Geena ; Chau, Terence
2026-02-01·JOURNAL OF SHOULDER AND ELBOW SURGERY
Does immobilization of patients who underwent a reverse total shoulder arthroplasty for proximal humerus fracture affect postoperative outcomes?
Article
作者: Fedorka, Catherine J ; Hedden, Kathryn ; Tornberg, Haley ; Millstein, Ian ; Derector, Evan ; Koneru, Manisha
HYPOTHESIS AND BACKGROUND:
Reverse total shoulder arthroplasty (rTSA) has become an increasingly popular treatment option for proximal humerus fractures (PHFs) in older patients. However, postoperatively, there lacks a universal protocol for the duration of arm immobilization in a sling. This retrospective review aims to determine whether the clinical outcomes of patients treated at our institution varied depending on their immobilization status following rTSA for PHF.
METHODS:
All patients aged >50 years with a diagnosis of PHF who were treated with rTSA at a level 1 trauma center between August 2016 and August 2023 with a minimum of 1-year follow-up were included. Patients were grouped into 2 cohorts based on postoperative immobilization. The early range of motion (EROM) cohort was allowed to use the sling for comfort and perform activities of daily living (ADLs) immediately postoperatively, whereas the immobilization cohort consisted of patients instructed to remain immobilized in the sling for 4-6 weeks. The duration of mobilization was recorded. Additional variables collected include demographics, preoperative comorbidities, Neer classification, range of motion (ROM), patient-reported outcomes, postoperative complications, tuberosity healing, and time to tuberosity healing.
RESULTS:
Of the 104 patients included in this study, 75 patients (72%) were immobilized in a sling and 29 patients (28%) were prescribed EROM postoperatively. Compared with the immobilization cohort, EROM patients had significantly better active abduction at 6 weeks (P = .011) and 12 weeks (P = .015) and active external rotation at 12 weeks (P = .013). There were no differences in ROM at the 6-month or 1-year follow-up and no differences in rates of tuberosity healing, patient-reported outcomes, or postoperative complications.
CONCLUSION:
Patients prescribed EROM following rTSA for PHF were found to have a faster recovery of ROM but no difference in any outcome at 1 year postoperatively. Complication and reoperation rates as well as tuberosity healing also did not differ between the 2 cohorts, further supporting EROM as a safe and effective option following rTSA. EROM allows patients to resume ADLs sooner, enabling a sense of independence in early recovery.
2026-01-01·OBSTETRICAL & GYNECOLOGICAL SURVEY
ESGO/INCIP Guidelines for the Management of Patients With Gynecological Cancers During Pregnancy
Review
作者: Lambertini, Matteo ; Vincent, Vandecaveye ; Hjortshøj, Cristel S. ; Amant, Frédéric ; McCluggage, W. Glenn ; Versteeg, Carolien ; De Middelaer, Anne ; Berveiller, Paul ; Fruscio, Robert ; Van Assche, Indra A. ; LeJeune, Charlotte L. ; Sienko, Jacek ; Poortmans, Philip ; Lok, Christianne ; Swierczynska, Marta ; Johansson, Anna L.V. ; Zapardiel ; Fumagalli, Monica ; Planchamp, François ; Testa, Antonia Carla ; Van Calsteren, Kristel ; Halaska, Michael J. ; Cardonick, Elyce ; Zagouri, Flora
Gynecological cancer requiring management during pregnancy is rare, with an estimated incidence of 2 to 5 per 100,000 pregnancies in the first trimester. Balancing maternal and fetal health in these cases can be difficult, and management strategies differ from nonpregnancy cases. Management strategies are typically determined by maximizing benefit to the mother while minimizing harm to the fetus, considering the extent of the cancer, available treatment options for each type of cancer, and the gestational age of the fetus. This article is a guideline presenting the highest standard of evidence for the management of these cases, although the authors recognize that following these recommendations is not always possible in all areas of the world. These guidelines address imaging, pathology, surgery, medical oncology, obstetrics, radiation therapy, psychology, patient perspective, and pediatric follow-up for ovarian, cervical, and vulvar cancers during pregnancy.The guidelines in this article were developed using the European Society of Gynecological Oncology (ESGO) via the ESGO Guideline Committee. This consists of a multidisciplinary international development group that uses scientific evidence and expert consensus, as well as an external international review process. A systematic review was performed as part of the creation of these guidelines, including relevant studies published between January 2014 and June 2024. In cases where evidence was unclear, professional experience and expertise were used to fill the gap.General guidelines included discussing treatment with a multidisciplinary team, patient and partner counseling being a priority (including diagnostic and treatment plans, potential alternatives, risks and benefits, and side effects), workup and treatment being conducted at a specialized center, patients receiving care as close as possible to nonpregnant patients, taking into account individual modifications as necessary, prioritizing research with these cases, and registration of all cancer cases during pregnancy. The incidence of cancer during pregnancy is not decreasing, and thus, practitioners should be aware of these possible complications of pregnancy. Recommendations include investigating symptoms of cancer immediately and thoroughly, as well as preserving the pregnancy because pregnancy does not worsen the prognosis of gynecological cancers.Imaging guidelines include ultrasound examination for diagnosis, with the reassurance of its safety during pregnancy, magnetic resonance imaging (MRI) for inconclusive ultrasound examination, referral to an experienced radiologist, repeated ultrasound examination for management planning, using ultrasound to evaluate patient response to neoadjuvant chemotherapy, and avoiding the use of gadolinium-based contrast agents, using diffusion-weighted MRI instead. In addition, the use of a lead apron for shielding is not recommended.The recommendations surrounding pathology include recording all relevant information on the pathology request form, referral for specialist opinion, and submission of the placenta for pathological examination after delivery. Surgical recommendations include locoregional anesthesia as a preferred method over general anesthesia and using a left lateral tilt of at least 15 degrees after 20 weeks of gestation. If procedures cannot be postponed, they should be performed during pregnancy even with an elevated risk to the fetus, though trauma to the uterus should be avoided. Minimally invasive procedures are preferred during pregnancy, when possible, though there is little evidence surrounding safe lengths and abdominal pressures; thus, surgical times and abdominal pressure should be minimized.Medical oncology guidelines include assessment of maternal and fetal health before each chemotherapy cycle, choosing a chemotherapy regimen based on cancer type, adapting standard treatment due to anticipated fetotoxic effects, and timing of chemotherapy to be after 12 weeks of gestation and before 35 weeks of gestation. In terms of obstetrics, it is recommended to encourage the use of compression stockings or devices during surgery and prophylactic low-molecular-weight heparin both after surgery and after delivery. Preterm birth should be avoided if possible, and delivery should be timed 2 weeks after the last course of chemotherapy if possible. If preterm delivery is expected, corticosteroids should be administered for fetal lung development in accordance with standard care recommendations. Cesarean delivery is recommended in cases of vulvo-vaginal cancer in situ and invasive cervical cancer, and vaginal delivery can be considered in cases where cancer has been completely removed or is restricted to the ovaries.The effects of radiation should be considered in a risk/benefit assessment for this therapy during pregnancy, and pelvic or groin radiation therapy should not be performed if pregnancy preservation is desired. Limited delay of radiation therapy should be considered if it allows for standard treatment, but minimizing fetal exposure can be considered as well in urgent cases. If pregnancy preservation is not desired, radiation therapy in combination with feticide or uterine evacuation can be proposed.Oncopsychologists should be included in the multidisciplinary team managing cases of gynecological cancer in pregnancy, and regular screening should be performed along with support offered at every stage of treatment during and after pregnancy. Patients and their partners should be included in treatment decisions and educated and consulted about their care. Long-term monitoring is recommended for children exposed to chemotherapy or radiation in utero, including assessments of hearing, cardiotoxicity, and neurodevelopmental delays.
4
项与 The Cooper Health System, Inc. 相关的新闻(医药)2025-07-14
Company also announces new 500-patient SUMMIT RISE study at the Society of NeuroInterventional Surgery annual meetingSAN MATEO, Calif., July 14, 2025 (GLOBE NEWSWIRE) -- Route 92 Medical, Inc., a privately held medical technology company dedicated to improving outcomes for patients undergoing neurovascular intervention, today announced results from an independent, real-world study evaluating reperfusion outcomes following use of Route 92 Medical’s HiPoint® Reperfusion System, the first and only FDA-cleared 0.088” reperfusion catheter system for direct aspiration of large vessel occlusions in patients experiencing an acute ischemic stroke. The study will be presented today by Daniel Tonetti, M.D., M.S., Director, Cerebrovascular Neurosurgery, Cooper University Health Care, at the Society of NeuroInterventional Surgery 22nd Annual Meeting being held in Nashville, Tennessee.
The retrospective, multicenter study collected outcomes data from 193 consecutive patients treated with Route 92 Medical’s HiPoint Reperfusion System who were not part of the SUMMIT MAX trial. The primary endpoints were first-pass effect of mTICI 2c/3 (a measure of clot removal) and first-pass effect, defined as mTICI 2b/2c/3 reperfusion on the first aspiration pass, with secondary endpoints including rate of successful aspiration catheter delivery, number of passes for final reperfusion, and conversion to other systems or devices.
Key study findings include:
Clinicians successfully delivered the HiPoint Reperfusion System to the stroke-causing occlusion in 96.2% of cases.The primary endpoint of first-pass effect mTICI 2c/3 was achieved in 57.5% of cases.The primary endpoint of first-pass effect of mTICI 2b/2c/3 was achieved in 68.4% of cases.Median number of passes was 1.
“We believed it was important to study the clinical utility of Route 92 Medical’s HiPoint Reperfusion System as a first-line aspiration tool in a real-world environment,” said Dr. Tonetti. “As in SUMMIT MAX and in the SLIC publication, we observed strong delivery and first pass effect data, as well as low complication rates. We’d expect these metrics to continue to improve as more clinicians and sites gain experience with the technology.”
Route 92 Medical also introduced SUMMIT RISE, a prospective 500-patient study to evaluate the efficacy of Route 92 Medical’s portfolio of neurovascular interventional solutions across a wide range of cases. The prospective, core-lab-adjudicated study will begin immediately under the leadership of co-primary investigators Sunil Sheth, M.D., Associate Professor and Director, Vascular Neurology Program at the McGovern Medical School at University of Texas, Houston, Christopher Kellner, M.D., Neurosurgeon at Mt. Sinai Health System, and Albert Yoo, M.D., Medical Director and Director of Research and Technology, Medical City Texas Stroke Institute.
“As with all new medical technologies, it’s critically important to develop independent, real-world evidence to guide future clinical decision-making,” said Dr. Sheth. “By collecting and analyzing data prospectively and having all cases reviewed through an independent adjudication process, the SUMMIT RISE study will enable us to evaluate the effectiveness of Route 92 Medical’s neurovascular interventional devices in real world clinical use and provide insights into technique optimization and performance.”
“We believe the evidence base supporting the use of Route 92 Medical’s technologies in neurovascular interventional procedures continues to grow. With each new study, there is additional support for the use of our Tenzing-based intervention approach, showing its ability to safely and effectively reach and aspirate clots, while improving first-pass effect relative to other catheter products,” said Tony Chou, M.D., founder and Chief Executive Officer at Route 92 Medical. “With SUMMIT RISE, we plan to evaluate patient outcomes over time, across devices and sites, and to provide additional data showing that our tools achieve clinical objectives and help give patients the best opportunity to recover from acute ischemic stroke.”
The HiPoint Reperfusion System is comprised of the HiPoint 88 Reperfusion Catheter, Tenzing® 8 Delivery Catheter, HiPoint 70 Reperfusion Catheter, Tenzing 7 Delivery Catheter, and Base Camp® 2.0 Sheath. It features the Monopoint approach, a streamlined telescoping design that advances from a single point of control. The Tenzing-powered delivery is designed to facilitate atraumatic navigation through tortuous anatomy, offering clinicians the flexibility to deliver vessel-matched, large- and super-bore catheters to the M1 and the ICA/ICA-T occlusions, while enabling the rapid and efficient removal of large vessel occlusions, the cause of many acute ischemic strokes.
There are approximately 800,000 total ischemic stroke episodes in the United States each year, 87% of which are ischemic strokes, in which blood flow to the brain is blocked.1 Despite recent advances in stroke treatment, stroke remains the leading cause of serious long-term disability and remains the fifth leading cause of death in the United States, responsible for approximately 163,000 deaths annually.2
To learn more, visit www.r92m.com.
About Route 92 Medical, Inc.Route 92 Medical is on a mission to improve outcomes for acute ischemic stroke patients undergoing neurovascular intervention and reduce suffering for these patients and their families by consistently reaching the clot, increasing first pass effect rates and simplifying the procedure with our systems. Founded by physicians, the company collaborates with leading neurovascular clinicians to solve the biggest challenges in neurointervention and deliver meaningful, differentiated solutions that promote clinical success. For more information, visit www.r92m.com or follow the company on LinkedIn.
1 Stroke Facts. U.S. Centers for Disease Control. Available: https://www.cdc.gov/stroke/data-research/facts-stats/index.html. Accessed May 15, 2025.2 Cerebrovascular Disease or Stroke. U.S. Centers for Disease Control, National Center for Health Statistics. Available: https://www.cdc.gov/nchs/fastats/stroke.htm. Accessed May 15, 2025. Contacts:
For Media
Gwen Gordon
858-245-5684
gwen@gwengordonpr.com
临床结果临床研究
2025-07-01
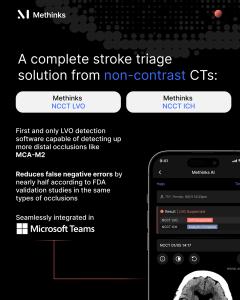
It is the first and only LVO detection software capable of detecting LVOs up to the MCA-M2 level using NCCT
Stroke remains a leading cause of disability and death worldwide, and timely treatment initiation is critical to improving patient outcomes. Methinks NCCT Stroke is a game-changer.”
— Tudor Jovin, MD, Chair of Neurology at Cooper University Health Care
BARCELONA, SPAIN, July 1, 2025 /
EINPresswire.com
/ -- While reducing false-negative errors by nearly half according to FDA validation studies.
Methinks AI
, a pioneer in AI-driven radiological triage and acute care coordination, announces that its Methinks NCCT Stroke software has received clearance from the U.S. Food and Drug Administration (FDA). This advanced software enhances the capabilities of non-contrast CT (NCCT) detection, becoming the only software on the market capable of detecting suspected Large Vessel Occlusions (LVOs) including more distal occlusions such as those in the MCA-M2 segment with high precision.
According to FDA validation studies, Methinks’ NCCT Stroke software delivers superior accuracy in detecting suspected LVOs reducing false-negative errors by nearly 50% compared to the most accurate NCCT LVO triage tool currently available for the same occlusion types. This is a crucial landmark in stroke care, as it reliably contributes to faster transfer and treatment decisions. The software also detects suspected intracranial haemorrhages (ICH), offering a comprehensive stroke triage solution with a routine NCCT scan, readily available in virtually any hospital.
This FDA 510(k) clearance significantly advances acute care workflows in the U.S. and globally. It reinforces Methinks AI’s commitment to expanding access to advanced stroke assessment and treatment using the most widely available imaging modality.
Methinks NCCT Stroke delivers breakthrough performance in detecting both suspected LVOs from standard NCCT scans, including those in the middle cerebral artery (MCA) segment M1 and the internal artery (ICA), as well as more distal occlusions in the MCA-M2 segment, and intracranial haemorrhages (ICH).
Uniquely integrated into Microsoft Teams, the solution enables real-time image sharing and clinical collaboration across stroke teams on a secure, widely adopted platform. This end-to-end system supports faster decisions, improved coordination, and optimizes stroke workflows — critical when every minute counts. Results also integrate smoothly into PACS and hospital workflows.
The Methinks solution can be deployed in any hospital, including those without contrast CT capabilities or advanced imaging. This helps reduce door-to-decision times, minimize delays in patient transfer or treatment initiation, and ensure that no stroke case is missed. This capability has far-reaching impact, especially in regional areas and healthcare settings with limited access to specialized stroke care, in the U.S. and worldwide.
METHINKS NCCT STROKE EMPOWERS GLOBAL ACCESS TO STROKE TREATMENT
“Achieving FDA clearance is a defining moment for our mission and our team,” said Pau Rodríguez, CEO of Methinks AI. “No patient should be left behind due to decision delays or limited imaging resources, whether in the U.S., Europe, or anywhere in the world. Methinks NCCT can unlock life-saving decisions at any hospital, bringing advanced stroke triage to every corner of the globe.”
“Methinks NCCT Stroke brings advanced LVO detection to hospitals everywhere, whether in the United States, Europe, or regions with limited imaging resources. This kind of innovation could significantly shorten the time to treatment and ultimately save lives by ensuring that stroke patients get the care they need as quickly as possible,” said Tudor Jovin, MD, Chair of Neurology at Cooper University Health Care and member of Methinks AI’s Board of Directors.
Microsoft Teams is already widely used in hospitals across the U.S., and Europe, and Methinks AI’s cloud-based infrastructure, deployed in Azure, reinforces global scalability. It offers seamless compatibility with any CT scanner worldwide, along with secure, scalable and workflow-friendly implementation options for healthcare providers around the world.
The new clearance arrives two months after Methinks AI announced a strategic partnership with
Medtronic
, the leading global healthcare technology company, to integrate Methinks’ triage software with Medtronic’s neurovascular portfolio. This collaboration will streamline stroke workflows across hospitals in Central and Eastern Europe, Africa, Türkiye and Middle East.
About Methinks AI
Founded in 2016, Methinks AI is a commercial-stage, VC-backed digital health company specializing in AI-powered imaging assessment solutions for neurovascular emergencies. Its mission is to provide universal and timely medical assistance through advanced, accessible technology. Methinks AI is the first company to receive
CE mark
for AI-based LVO assessment support on non-contrast CT. This achievement contributes to the evolution of early stroke care globally.
Methinks Press
Methinks AI
+34 935 41 41 86
email us here
Visit us on social media:
LinkedIn
YouTube
X
Other
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability
for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this
article. If you have any complaints or copyright issues related to this article, kindly contact the author above.
2024-07-01
The closing is complete and Cape Regional Health System is now part of Cooper University Health Care, effective today, July 1, 2024. As part of the closing, Cape Regional Medical Center has been renamed Cooper University Hospital Cape Regional.
"This agreement will transform health care for the residents and visitors of Cape May and Atlantic counties,” said George E. Norcross III, Chairman of Cooper University Health Care’s Board of Trustees.
“We are ready to move forward and for our unified team to begin delivering the highest level of advanced health care to more people in shore communities and beyond. We are excited by the opportunity to build something extraordinary here.”
“Today is a significant day and a new chapter for health care in Cape May County and beyond. I want to thank our entire team for all the great work in serving the people of this community so well, for so many years, that brought us to this exciting new beginning where we will be able to serve even more people,” stated Garry Gilbert, former Chairman, Cape Regional Health System Board of Trustees.
In December 2022, Cooper and Cape Regional announced the proposal to join together, followed by execution of a Definitive Agreement in April 2023. Final regulatory approval by the New Jersey Superior Court of Cape May County was secured on May 28, 2024. The transaction was officially completed effective today.
Cooper, with its market-leading MD Anderson Cancer Center at Cooper, is based in the City of Camden and is southern New Jersey’s leading academic health system and only Level I trauma center, with more than $2.2 billion in revenue. Cape Regional Health System has earned the Gold Seal of Approval from the Joint Commission and is an integrated health care delivery system serving residents throughout Cape May County.
“We are happy to have brought this vision to reality. We look forward to working with our new colleagues to build upon their tremendous work and provide the highest quality of primary and specialty care to the residents and visitors at the shore,” said Anthony J. Mazzarelli, MD, JD, MBE, co-CEO of Cooper University Health Care.
“Today is a day of great promise, as two teams have become one team dedicated to serving communities across South Jersey,” said Kevin O’Dowd, JD, co-CEO of Cooper University Health Care. “We look forward to the future and the work we will do with our new team members and with residents and visitors to the shore region.”
“The future of health care is very bright for the residents and visitors of Cape May County as a result of this merger,” stated Joanne Carrocino, FACHE, CEO, Cooper University Hospital Cape Regional. “The Cape Regional team is excited to begin working with our new colleagues at Cooper.”
“The entire Cooper team is looking forward to collaborating with our new team members in Cape May County to enhance access to the highest levels of care and enrich the health care experience for the people of Cape May and Atlantic counties,” said Christine Winn, PhD, FACHE, Senior Vice President and Chief Regional Officer for Cooper, who will oversee Cooper operations in Cape May and Atlantic counties, including Cooper University Hospital Cape Regional.
并购
100 项与 The Cooper Health System, Inc. 相关的药物交易
登录后查看更多信息
100 项与 The Cooper Health System, Inc. 相关的转化医学
登录后查看更多信息
组织架构
使用我们的机构树数据加速您的研究。
登录
或

管线布局
2026年02月09日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床前
1
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

转化医学
使用我们的转化医学数据加速您的研究。
登录
或

营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或

科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或

融资
发掘融资趋势以验证和推进您的投资机会。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用

