预约演示
更新于:2026-02-07
Renadirsen
更新于:2026-02-07
概要
基本信息
药物类型 ASO |
别名 duchenne muscular dystrophy therapeutics - Daiichi Sankyo/Orphan Disease Treatment Institute、ENA oligonucleotides、DS-5141 + [1] |
作用方式 调节剂 |
作用机制 DMD基因调节剂 |
在研适应症 |
非在研适应症- |
非在研机构- |
权益机构- |
最高研发阶段临床2期 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
结构/序列
使用我们的RNA技术数据为新药研发加速。
登录
或
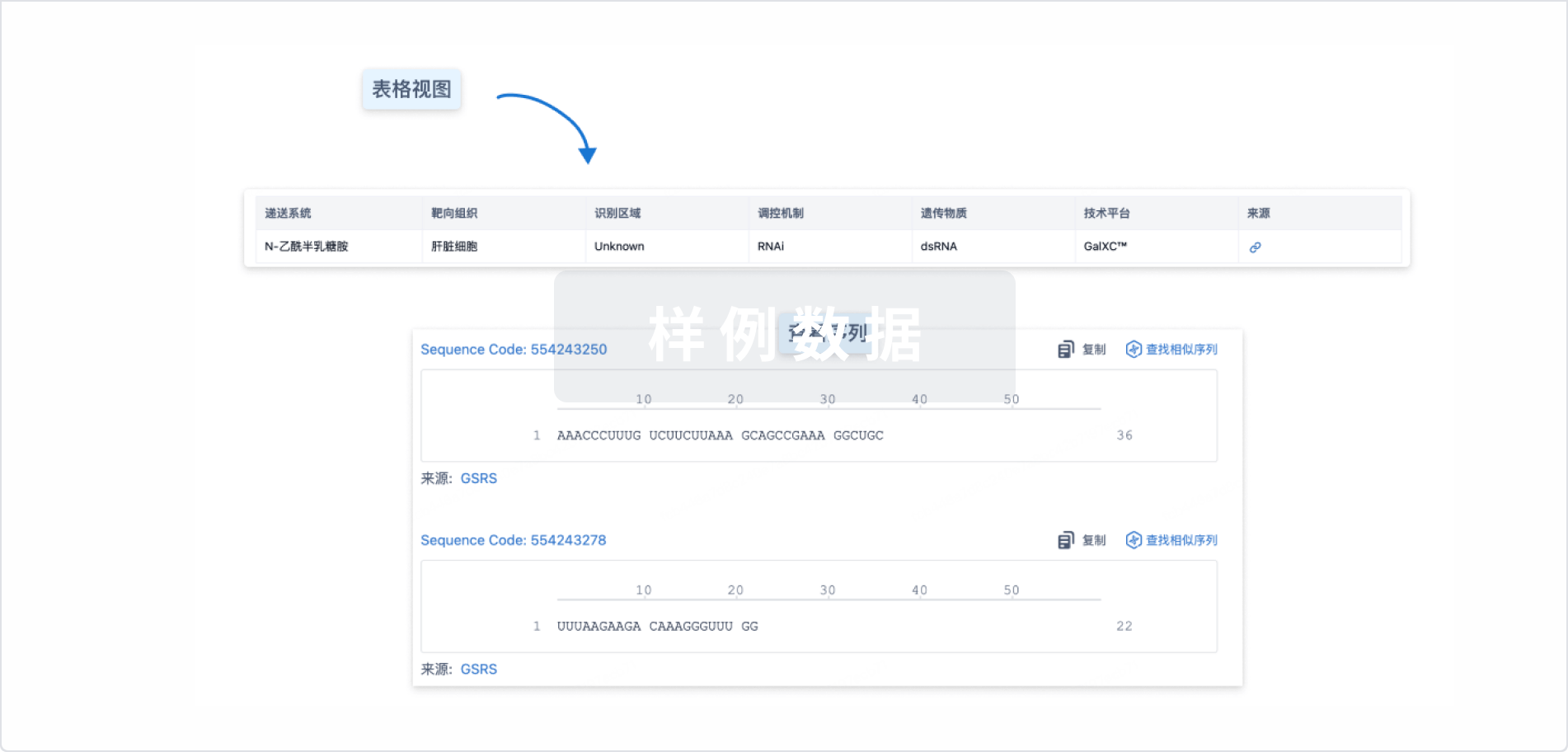
Sequence Code 32858997

来源: *****
关联
2
项与 Renadirsen 相关的临床试验NCT04433234
A Phase II, Long-term, Extension Study of DS-5141b in Patients With Duchenne Muscular Dystrophy
This is a multicenter, open-label, long-term, extension, phase 2 study to evaluate the safety and efficacy of long-term treatment with DS-5141b in patients with DMD who have completed DS5141-A-J101.
开始日期2020-06-30 |
申办/合作机构 |
NCT02667483
Phase I/II Study of DS-5141b: Open-label Study of DS-5141b in Patients With Duchenne Muscular Dystrophy
This is a phase I/II study to evaluate the safety, tolerability, efficacy, and pharmacokinetic (PK) profile of DS-5141b in patients with Duchenne muscular dystrophy (DMD) amenable to exon 45 skipping and to determine the dosage for subsequent studies.
开始日期2015-10-01 |
申办/合作机构 |
100 项与 Renadirsen 相关的临床结果
登录后查看更多信息
100 项与 Renadirsen 相关的转化医学
登录后查看更多信息
100 项与 Renadirsen 相关的专利(医药)
登录后查看更多信息
2
项与 Renadirsen 相关的文献(医药)2025-08-03·NUCLEOSIDES NUCLEOTIDES & NUCLEIC ACIDS
Tissue distribution of renadirsen sodium, a dystrophin exon-skipping antisense oligonucleotide, in heart and diaphragm after subcutaneous administration to cynomolgus monkeys
Article
作者: Yamamura, Naotoshi ; Takaishi, Kiyosumi ; Asano, Daigo ; Kanda, Akira ; Yamanaka, Ryo ; Takeshima, Yasuhiro ; Shibaya, Yukari ; Takakusa, Hideo ; Koizumi, Makoto ; Watanabe, Kyoko ; Matsuo, Masafumi ; Fusegawa, Keiichi ; Nagase, Hiroyuki
The pharmacokinetics and tissue distribution of renadirsen sodium, a dystrophin exon-skipping phosphorothioate-modified antisense oligonucleotide with 2'-O,4'-C-ethylene-bridged nucleic acid (ENA), after subcutaneous or intravenous administration to cynomolgus monkeys were investigated. The plasma concentration of renadirsen after subcutaneous administration at 1, 3, and 10 mg/kg increased with the dose. The absolute bioavailability at 3 mg/kg after subcutaneous administration was calculated as 88.6%, and the time to reach maximum plasma concentration of renadirsen was within 4 h, indicating the efficient and rapid absorption following subcutaneous administration. The exposure of muscle tissues to renadirsen was found to increase with repeated dosing at 6 mg/kg, and higher exposure was observed in the diaphragm and heart than in the quadriceps femoris and anterior tibialis muscles. Renadirsen achieved more exon 45-skipped dystrophin mRNA in the diaphragm and heart than in the quadriceps femoris and anterior tibialis muscles. Renadirsen also showed a cumulative skipping effect in a repeated-dose study. The findings on exon 45-skipped dystrophin mRNA in these muscle tissues were consistent with the concentration of renadirsen in these tissues. Because it is not feasible to directly evaluate drug concentration and exon skipping in the heart and diaphragm in humans, the pharmacokinetics and pharmacodynamics of renadirsen in these tissues in monkeys are crucial for the design and interpretation of clinical settings.
Current issues in molecular biology4区 · 生物学
Renadirsen, a Novel 2′OMeRNA/ENA® Chimera Antisense Oligonucleotide, Induces Robust Exon 45 Skipping for Dystrophin In Vivo
4区 · 生物学
Article
作者: Masuda, Takeshi ; Asano, Daigo ; Takaishi, Kiyosumi ; Takakusa, Hideo ; Ito, Kentaro ; Goda, Ryoya ; Kakuta, Masayo ; Onishi, Yoshiyuki ; Onoda, Toshio ; Nakamura, Akifumi ; Takagi, Nana ; Koizumi, Makoto ; Takeshima, Yasuhiro ; Nagase, Hiroyuki ; Watanabe, Nobuaki ; Matsuo, Masafumi ; Kanda, Akira
Duchenne muscular dystrophy (DMD) is a progressive muscle-wasting disease caused by out-of-frame or nonsense mutation in the dystrophin gene. It begins with a loss of ambulation between 9 and 14 years of age, followed by various other symptoms including cardiac dysfunction. Exon skipping of patients’ DMD pre-mRNA induced by antisense oligonucleotides (AOs) is expected to produce shorter but partly functional dystrophin proteins, such as those possessed by patients with the less severe Becker muscular dystrophy. We are working on developing modified nucleotides, such as 2′-O,4′-C-ethylene-bridged nucleic acids (ENAs), possessing high nuclease resistance and high affinity for complementary RNA strands. Here, we demonstrate the preclinical characteristics (exon-skipping activity in vivo, stability in blood, pharmacokinetics, and tissue distribution) of renadirsen, a novel AO modified with 2′-O-methyl RNA/ENA chimera phosphorothioate designed for dystrophin exon 45 skipping and currently under clinical trials. Notably, systemic delivery of renadirsen sodium promoted dystrophin exon skipping in cardiac muscle, skeletal muscle, and diaphragm, compared with AOs with the same sequence as renadirsen but conventionally modified by PMO and 2′OMePS. These findings suggest the promise of renadirsen sodium as a therapeutic agent that improves not only skeletal muscle symptoms but also other symptoms in DMD patients, such as cardiac dysfunction.
6
项与 Renadirsen 相关的新闻(医药)2023-07-10
·药融圈
▲8月03-04日 CMC-China大会 · 限时免费扫码报名中注:本文不构成任何投资意见和建议,以官方/公司公告为准;本文仅作医疗健康相关药物介绍,非治疗方案推荐(若涉及),不代表平台立场。任何文章转载需得到授权。管线消失,但带给我们的启示不会消失。他山之石,可以攻玉。跨国药企在创新方面一直走在前列,其管线项目的布局调整,值得我们密切关注。据不完全统计,上半年辉瑞、BMS、诺华、罗氏、默沙东、GSK、武田、阿斯利康、第一三共等大药企合计砍掉了超50个管线项目,涉及ADC、CGT疗法、新冠药物、小核酸、疫苗和GLP-1等各个方面,或因为技术不成熟,难成药;或由于竞争格局发生变化以及战略失误等原因,我们具体来看看。辉瑞在2023年上半年终止10多个研发项目。今年2月初,辉瑞发布的财报显示,消减了8个研发项目。1.删掉了recicept研发项目,这是一种治疗软骨发育不全的侏儒症的药物,是辉瑞在2019年收购罕见疾病公司Therachon的核心产品。当时,辉瑞公司预付了3.4亿美元。2.削减两个Paxlovid的适应症,这两个适应症在各自的III期试验中都失败了——一个用于标准风险患者,一个用于暴露后预防。3.停止了四种早期候选药物的研发,其中包括一种正在健康志愿者身上测试的治疗自身免疫性疾病的药物。该药被授予孤儿药称号,用于治疗一种称为慢性炎症性脱髓鞘多发性神经病的神经疾病。此外,该公司正在开发一种用于实体瘤的生物制剂,以及用于黑色素瘤和转移性乳腺癌的激酶抑制剂。辉瑞在年初时候表示,将缩小对罕见疾病和癌症的关注,未来计划在血液学和基因编辑等目前的重点领域加大投入。2023年5月初,辉瑞在一季报中更新了其研发管线,其中有6个研发项目已终止,101个项目仍处于临床或注册阶段。图片来源:辉瑞官网辉瑞公司还在1季报中披露了自1月31日以来剔除的6个研发项目,如下图所示:来源:官网BMS在2023年2月发布的财报显示,至少9个管线被砍,包括CTLA-4和TIGIT等靶点。其中在早期研发方面,BMS削减了6项肿瘤资产,包括一项2期抗CTLA-4候选药物BMS986218、一项纤维化候选药物和两项免疫学资产。大多数肿瘤资产为1期实体瘤管线,包括STING激动剂、IL-12 F、SIRPα拮抗剂和anti-CTLA-4药物。此外,BMS也削弱了其血液瘤的前景,终止了处于1期的ROR CAR-T疗法的开发,同时BMS还终止抗TIGIT药物BMS-986207的2期临床试验,该试验是Yervoy和Opdivo三联疗法的一部分,主要是出于安全考虑。罗氏在2023年2月财报显示,12款产品减值超31亿美元。2022年资产减值超31美元,涉及12款主要产品,其中最大的一笔是抗癌药物Gavreto减值7.26亿美元,这是一种口服RET靶向疗法,用于治疗年龄≥12岁的甲状腺癌儿童和成人患者。此外,2022年罗氏在基因疗法方面资产减值金额约7.5亿美元。2023年5月,罗氏终止精神病新药II期临床研究。美国临床试验网显示,罗氏终止了其精神分裂症候选药物ralmitaront的II期(NCT03669640)临床试验,该研究旨在评估ralmitaront相较于安慰剂用于治疗精神分裂症或分裂情感障碍阴性症状患者疗效。试验终止的原因是中期分析表明ralmitaront不太可能在该研究中达到主要终点。2023年6月,据媒体报道,罗氏将终止推进反义寡核苷酸疗法rugonersen治疗天使综合征的临床开发。罗氏表示,该疗法的耐受性良好,这一决定无关安全性问题。停止rugonersen开发的决定并不意味着罗氏放弃天使综合征领域。罗氏补充说,正在进行的alogabat治疗天使综合征的II期研究将不受影响。该小分子是一款GABRA5正向变构调节剂。默沙东停止3个项目。据2月份发布的财报更新显示,默沙东公司放弃了基孔肯雅热(chikungunya)候选疫苗,该疫苗已完成II期研究。默沙东公司于2020年通过收购Themis Bioscience 获得了该疫苗。此外,默沙东还放弃了Lenvima的胶质母细胞瘤适应证,该公司一直在研究Lenvima与Keytruda联合用于LEAP项目的适应证。在一封电子邮件中,默克公司告诉Endpoints News:“作为我们常规管道优先排序的一部分,MSD已经选择停止这两个项目。”在1月25日,MSD宣布,在一项中期分析显示生存率没有改善后,MSD还将停止一项Keytruda晚期前列腺癌研究。GSK在2月份发布的财报显示,删除2个项目。GSK从其管线中删除了一种名为GSK3915393的化合物。该化合物可抑制一种称为转谷氨酰胺酶2或TG2的酶,该公司此前一直在研究其在乳糜泻中的应用。当在媒体电话会议上被问及3915393计划时,首席执行官Emma Walmsley证实没有进一步的计划来测试该药物是否用于乳糜泻。另外,GSK也在放弃一种针对金黄色葡萄球菌的重组蛋白疫苗,该疫苗已进入第二阶段。年初GSK还指出,它“决定停止对细胞和基因疗法的投资,最显著的是,本着在研发方面“极其严格”的精神,断绝了与Lyell、Adaptimmune和Immatics的联盟。武田在2023年5月披露的财报显示,终止6个研发项目。1.TAK-954。武田将放弃II期临床试验失败的术后胃肠功能障碍候选药物TAK-954。这是一款选择性5-HT4受体激动剂,从爱尔兰公司Theravance Biopharma授权引进,由此也结束了两家公司之间的合作。2.TAK-018(sibofimloc)。sibofimloc是一款与法国Enterome Biosciences公司合作开发的FimH 粘附抑制剂,用于克罗恩病(CD)。此款药物终止研发的原因是因为未能招募到足够的患者进行II期试验。3.Ninlaro (ixazomib)。Ninlaro是FDA批准的首个口服蛋白酶体抑制剂,用于治疗复发性或难治性多发性骨髓瘤(R/R MM)。根据研究的最终分析,武田决定停止在美国和欧洲开发新的适应症——治疗首次发作的多发性骨髓瘤,而无需造血干细胞移植。4.LIVTENCITY(马里巴韦)。在与监管当局审查了试验结果后,武田停止了该药物在造血干细胞移植后巨细胞病毒感染的一线治疗适应症的开发。5.Taxilo。该药物在缓激肽介导的血管性水肿研究中未能达到其主要终点。6.Zejura (niraparib)。武田停止Zejura在乳腺癌研究中的患者招募。Zejura是一款PARP抑制剂,目前用于卵巢癌。第一三共终止了2个研发项目。2023年5月份,第一三共发布2022财年(2022年4月1日-2023年3月31日)财报显示,终止了2个研发项目。包括用于杜氏进行性肌营养不良(DMD)的核酸药物DS-5141和用于进行性骨化性纤维发育不良(FOP)的药物DS-6016DS-5141是一款有望治疗DMD的核酸药物,可以跳过45外显子拼接,在信使RNA的处理过程中,在肌细胞中产生不完整但具有功能的肌营养不良蛋白。虽然在临床试验中显示出了一定的有效性,但根据目前的数据判断,想要进一步开发比较困难。DS-6016是一款有望治疗FOP的抗ALK2抗体,由于需要花费时间解决相关抗体非临床试验中发现的潜在安全性风险,因此被判定失去了竞争力,所以终止了开发。阿斯利康砍掉2个GLP-1管线和IL-4Rα拮抗剂开发。2023年6月20日,据外媒fiercebiotech报道,阿斯利康AZD0186(GLP-1R激动剂)没有达到预期目标,未显示出足够的差异性以超过当前的护理标准,故决定终止这项临床研究AZD0186处于1期临床研究阶段,用于治疗2型糖尿病,此项研究主要评估AZD0186 的安全性、耐受性和药代动力学。除了AZD0186,4月12日,阿斯利康宣布放弃一项关于Cotadutide(GLP-1R/GCGR 双重激动剂、日制剂)的 IIb/III 期临床研究,针对伴有肝纤维化但无肝硬化的非酒精性脂肪肝炎(NASH)患者。Cotadutide数据疗效不错,但和已上市的几款药物相比,并不具备竞争优势。阿斯利康表示将重点开发另一款GLP-1R/GCGR激动剂AZD9550(周制剂),目前仍处于临床前开发阶段。6月21日,Pieris Pharmaceuticals宣布收到阿斯利康向其传达的终止elarekibep开发的决定。该决定基于一项为期13周的非临床GLP毒理学研究,与正在进行的临床研究无关,但研究结果不支持elarekibep的长期使用以及临床后期开发。除了跨国大药企砍管线以外,还有不少中小药企也在陆续砍管线,ADC领域也有知名公司砍管线。今年5月份,ADC Therapeutics也砍掉了2道ADC管线,分别是ADCT-212(治疗前列腺癌的临床前抗体药物结合物)和ADCT-701(靶向DLK-1的ADC药物)。ADC Therapeutics执行官补充说,临床前项目的削减将使公司有更多的资金用于上市产品Zynlonta和其后期临床项目。总结此外,据公开报道,强生上半年还搁置了2个“双抗管线”研发;诺华调整Cosentyx、CAR-T疗法、TIGIT 抗体等研发计划;吉利德暂停3个项目,包括IRAK4抑制剂的两个适应症以及一个实体瘤候选物;礼来放弃了一种治疗糖尿病和非酒精性脂肪性肝炎的第一阶段候选药物,赛诺菲也停止了对BTK抑制剂tolebrutinib用于重症肌无力(MG)的III期临床研究等项目,艾伯维也终止开发一款自免ADC药物ABBV-154。管线项目的消失提醒我们,在投入大量资源和精力之前,必须充分评估项目的可行性和潜在风险。这要求药企更加注重风险管理和决策的科学性,以减少研发过程中的失败率。参考资料:各公司官网https://endpts.com/news/https://www.fiercepharma.com/版权声明:本文转自药事纵横,如不希望被转载的媒体或个人可与我们联系,我们将立即删除关于CMC-China 博览会融合产业力量,重构行业未来!本次CMC-China博览会汇聚300+医药及上下游全产业链的企业积极报名参展,数千名专业观众报名参观,展会现场将举办15场专业论坛。充分体现了“医药人办医药展,专业人办专业展”的理念。了解更多:数据看展会丨一文看懂第五届CMC-China制药博览会观众亮点点分享点点赞点在看
财报免疫疗法孤儿药疫苗细胞疗法
2023-05-21
·药时代
编者按:2023 Q1,多家药企接连终止在研管线,例如,GSK结束对细胞基因疗法领域的投入、诺华削减10%非核心管线、武田放弃AAV基因疗法和罕见血液学领域……当然,也有例外,例如诺和诺德。在糖尿病与肥胖领域,其司美格鲁肽很有可能成为今年“药王”的有力竞争者。关于诺和诺德的研发之道,药时代有幸采访到了诺和诺德全球药物发现负责人,相信对致力于研发FIC药物的企业们会有帮助。百年药企诺和诺德如何「以慢制快」?对话诺和诺德全球药物发现高级副总裁 Karin Conde-Knape博士药时代对强生、礼来、艾伯维、罗氏、阿斯利康、辉瑞、BMS、赛诺菲、安进、再生元、拜耳、第一三共、渤健、GSK的四十多条终止管线进行了汇总梳理,在此与大家分享。小分子药物被砍掉最多小分子药物是被砍掉最多的类型,有20条管线。辉瑞一共终止了6条管线,其中5条为小分子药物,分别是:用于急性心力衰竭的APD418、用于血管阻塞的Temanogre、用于治疗雷诺氏综合征的Temanogrel、用于掌跖脓疱病和化脓性汗腺炎两种适应症的RIST4721。(图源:辉瑞官网)拜耳的4项终止均为小分子药物,分别为:用于糖尿病神经性疼痛的BDKRB1 受体拮抗剂、用于慢性肾病的Runcaciguat、用于子宫内膜异位症的BAY 2395840和P2X4拮抗剂。礼来终止TRPA1 拮抗剂在镇痛领域的研究;艾伯维终止ABBV-154在囊性纤维化上的研究;阿斯利康终止ALXN1840在威尔逊病领域的研究;BMS终止iberdomide在淋巴瘤上的研究;赛诺菲终止Tolebrutinib和atuzabrutinib在自身免疫病相关研究;渤健终止BIIB093在脑挫伤和大脑半球梗塞领域的研究,及BIIB131在急性缺血性中风上的研究;GSK停止了Zejula在乳腺癌领域的研究。(图源:Lilly官网)(图源:百时美施贵宝官网)单抗类药物次于小分子药物,被砍掉逾10条管线。罗氏一共终止了3条单抗类药物管线,均为Tecentrig组合药物,分别为:用于一线转移性尿路上皮癌的Tecentrig+chemo、用于二线非小细胞肺癌的Tecentriq+Cabometyx、用于二线her2阳性、PD-L1阳性转移性乳腺癌的Tecentriq +Kadcyla。赛诺菲和再生元均分别终止了Dupixent的一条管线,分别为过敏性真菌性鼻炎和无鼻息肉慢性鼻窦炎、慢性寒冷引起的荨麻疹。阿斯利康终止了用于实体瘤的AZD8853和用于一线转移性非小细胞肺癌的Imfinzi。礼来终止用于阿尔兹海默症的solanezumab;辉瑞终止用于溃疡性结肠炎的PF-06480605;BMS终止用于黑色素瘤的nivolumab +rHuPH20;第一三共终止用于进行性骨化性纤维发育不良的DS-6016。疫苗终止了两条管线,均为强生的药物,分别是成人RSV疫苗和HIV疫苗。反义寡核苷酸类药物共有两个,分别是第一三共用于杜氏进行性肌营养不良的DS-5141和渤健用于脊髓小脑性共济失调3型的BIIB132。融合蛋白类有两个,分别为礼来和安进用于系统性红斑狼疮的Rezpegaldesleukin和efavaleukin alfa。剩下的为阿斯利康用于NASH领域的合成多肽类药物cotadutide、罗氏用于骨髓纤维化的重组蛋白类药物zinpentraxin alfa、安进用于系统性红斑狼疮的双特异性抗体药物Rozibafusp alfa。免疫和肿瘤领域依然占大头被砍掉的自免型疾病管线占大头,有11条。其次是肿瘤类管线,有8条。再就是罕见病领域,有4条管线被终止。渤健终止的几条管线均为脑血管疾病领域。II期项目“夭折”最多根据统计,除去部分临床阶段不明的管线,在II期被终止的管线有19条:在III期被终止的管线有11条:在I期被终止的管线有6条:II期试验也称为疗效试验或临床效能试验。主要目的是评估新药在特定疾病人群中的治疗效果和安全性。如果在这个阶段没有足够的证据表明新药对疾病有明显的疗效,或者新药的效果与已有治疗方案相比没有显著优势,试验可能会被终止。同时,临床II期试验是在相对较大规模的患者群体中进行的,这时候药物的潜在安全性问题更容易被发现。如果药物出现了严重的安全问题,试验可能会被终止以保护患者安全。而III期实验的终止,可能是因为前两期的实验过程出现了问题,而导致潜在安全问题没有被发现。且即使是到了申报上市的阶段,也有可能管线被终止,而无法上市。只过了2个月,就从「即将获批」变成了「管线终止」......这款药,是从一开始就做错了吗?封面图来源:123rf2023年1月1日至今,~20笔中国新药出海交易横空出世,总金额高达上百亿美元!一时间,喜讯频传,令行业、企业和每一位同药振奋!曾经提出“百靶竞技,百炼创新,百家上市,百药争先”的药时代团队再一次真切感受到:中国新药研发正当时!中国新药出海正当时!中国新药BD正当时!在这个BD如火如的好时代里,企业对于BD的要求不断提高,如何与时俱进,学习最新BD知识,掌握最新BD技能,成为摆在每一位BD同药面前的一个实际而迫切的问题。为了帮助企业培养优秀的BD高级人才,为了帮助BD人才成长进步,药时代学苑全力打造创新药BD高级研讨会,致力于成为中国制药界ZUI有实力和活力的学习平台。点击这里,报名参加,一起快乐学习!
基因疗法细胞疗法
2023-04-27
·药智网
近两年,继小分子和抗体药物之后,小核酸药物也得到了人们的关注。小核酸药物是一种全新的药物类别,由核苷酸组成,主要作用于细胞质的mRNA,通过碱基互补识别和抑制靶mRNA,实现对蛋白表达的调控,达到治疗疾病的目的。经过几十年的基础研究,到目前为止共有15款小核酸药物获批上市,主要包括小干扰核酸(siRNA)、反义核酸(ASO)这两大类。小核酸药物之所以很重要,是因为它们可以克服传统药物或抗体的一些限制,如靶向难治性分子、特异性、稳定性和递送。然而,它们也面临一些挑战,如毒性、免疫原性和成本过高。因此,我们准备通过一系列文章来给博药的读者们介绍有关小核酸药物的相关资讯。01小核酸药物,小分子核苷类药物和mRNA疫苗在介绍一下小核酸药物之前为了避免混淆先比较一下三者的异同。 小核酸药物、小分子核苷类药物和mRNA疫苗都是基于核苷酸的药物或疫苗,但它们的作用机制和应用领域有所不同。 小核酸药物是指长度小于30nt的寡核苷酸序列,包括小干扰核酸(siRNA)、信使RNA(mRNA)、微小RNA(miRNA)、反义核酸(ASO)和核酸适配体(Aptamer)等。这些药物通过与靶分子的RNA结合,抑制其翻译或调控,从而达到治疗的效果。小核酸药物具有高度的靶向性和特异性,可以精准地调控基因表达,因此在基因治疗和基因编辑等领域具有广阔的应用前景。 而小分子核苷类药物是一类分子量较小的核苷酸类药物,通常用于治疗病毒感染和癌症等疾病。这些药物通过与病毒或癌细胞的DNA或RNA结合,抑制其复制和转录,从而达到治疗的效果。 mRNA疫苗是一种新型的疫苗,通过注射体内产生的mRNA编码病原体的抗原蛋白,从而激发机体免疫反应。近日首款国产新冠mRNA疫苗SYS6006获批紧急使用的新闻让我们再次关注mRNA技术。mRNA技术是一种利用人体细胞内的机制,将特定的遗传信息传递给细胞,从而诱导细胞产生所需的蛋白质或抗原的方法。不过mRNA疫苗需要在低温下保存和运输,增加了疫苗保存和运输的难度和成本。 表1:小核酸药物,小分子核苷类药物和mRNA疫苗的异同资料来源:根据公开资料整理02小核酸药物的发展历程小核酸药物的发展可以追溯到20世纪70年代,当时科学家发现了反义核酸antisense oligonucleotides(ASO)的作用机制。ASO是一种通过靶向特定基因的mRNA序列来抑制蛋白质表达的寡核苷酸。在1990年代,RNA干扰(RNAi)技术被发现,RNAi寡核苷酸可以通过干扰mRNA的降解和翻译来抑制基因表达。这一技术为开发新的基因治疗方法提供了新思路。此外,适配体寡核苷酸也在这一时期被发现,并被证明可以作为高度特异的药物靶标,具有很高的治疗潜力。随着基因测序和合成技术的不断发展,寡核苷酸药物的设计和制备变得越来越精准和高效。最近几年,随着mRNA疫苗的出现,寡核苷酸药物的发展进入了一个新的阶段。mRNA疫苗利用寡核苷酸的优良性质,通过传递编码抗原的mRNA分子来诱导免疫反应,成为了应对COVID-19等传染病的一种重要工具。下图总结了治疗用反义寡核苷酸的化学修饰演变历程。图1:小核酸药物跌宕起伏的发展历程。图片来源:参考资料1上世纪九十年代,ODNs和ORNs的各种修饰被研究,基于RNase H活性,PS-ODNs成为第一代反义试剂的选择。但很快发现,PS-ODN存在脱靶活性,如补体激活和序列特异性免疫激活,导致其作用机制和安全性受到质疑,大多数PS-ODN ASO的临床开发已停止。随后,ORN修饰的平行使用进行细胞中的剪接校正。gapmer反义设计基于九十年代初的早期工作,提供了关键属性,成为第二代反义试剂的选择。反义化学修饰的研究促进了其他治疗性寡核苷酸的开发。关键修饰已被确定,例如PS-PDN和PS-ORN,2'-修饰或2'-O-取代的核糖核苷、桥接核糖核苷和PMO,它们被用于各种核酸治疗。近年来,基于gapmer ONs(如mipomersen、inotersen、volanesorsen)、2'-MOE PS-ORN(如nusinersen)、PMO(如eteplirsen、golodirsen、vitolarsen)和siRNA(如patisiran、givosiran)的药物已获批准。03已获批的15款小核酸药物近年来,随着相关研究和技术的进步,小核酸药物迎来了快速的发展,全球上市的核酸药物数量逐年递增,截至目前全球共有15款小核酸药物在获批上市,这些药物主要用于治疗遗传性和罕见疾病,如杜兴氏肌肉萎缩症、脊髓性肌肉萎缩症、遗传性转甲状腺素淀粉样变性等。表2:全球已批准的小核酸药物汇总资料来源:根据公开资料整理技术路线分类包括反义核酸(ASO)、RNA干扰(RNAi)、CRISPR/Cas9等。其中,反义核酸ASO与靶mRNA精准互补,降解mRNA,从而阻断其翻译。目前全球有8款ASO药物获批上市,有超过50个ASO药物处于临床研究阶段。已批准ASO药物中有5个为Ionis研发,2个由Sarepta研发,1个由日本Shinyaku公司研发。除了欧美药企,我国的核酸制药业态也在不断发展。主要包括反义核酸、小干扰核酸、核酸适配体、小激活核酸、微小核酸、mRNA药物、核酶等。国内制药企业在研发方面也取得了一定的成果。例如,苏州瑞博生物获得了一款治疗糖尿病的二期产品GCGR反义核酸的中国权益转让。此外,日本的制药公司和生物创业公司也在开发具有自主技术的核酸药物,如Viltolarsen(Nippon Shinyaku)、DS-5141(Orphan Disease Treatment Institute)、STNM01(TME Therapeutics)等。目前开发设计小核酸药物的最大挑战是如何解决药物递送问题,或者通过化学改造核酸药物的成药性,长久以来小核酸类药物的稳定性一直是软肋。小核酸药物的创新药研发不仅要考虑核酸序列的专利,更多的是需要布局各种药物递送系统。04小结小核酸药物作为靶向RNA并调节基因表达或功能的药物具有三大特点:高度特异性、持久性和可治愈性。目前小核酸药物已经显示出治疗各种疾病的前景,特别是遗传性和罕见病。还有许多候选药物正在开发中,用于治疗常见疾病,如癌症、心血管疾病和病毒感染等。当然小核酸药物在药物递送过程中面临着稳定性、生物分布、细胞摄取、内体逃逸和免疫原性等挑战。目前新药研发团队已开发出各种策略来克服这些挑战,如化学修饰、生物偶联和纳米载体制剂。参考资料:1. Gait, M.J. and Agrawal, S., 2022. Introduction and History of the Chemistry of Nucleic Acids Therapeutics. In Antisense RNA Design, Delivery, and Analysis (pp. 3-31). New York, NY: Springer US.2. Igarashi, J., Niwa, Y. and Sugiyama, D., 2022. Research and development of oligonucleotide therapeutics in Japan for rare diseases. Future Rare Diseases, 2(1), p.FRD19.Moumné, L., Marie, A.C. and Crouvezier, N., 2022. Oligonucleotide therapeutics: from discovery and development to patentability. Pharmaceutics, 14(2), p.260.来源 | 博药(药智网获取授权转载)撰稿 | 费翔责任编辑 | 八角声明:本文系药智网转载内容,图片、文字版权归原作者所有,转载目的在于传递更多信息,并不代表本平台观点。如涉及作品内容、版权和其它问题,请在本平台留言,我们将在第一时间删除。商务合作 | 王存星 19922864877(同微信) 阅读原文,是昨天最受欢迎的文章哦
寡核苷酸信使RNA上市批准核酸药物siRNA
100 项与 Renadirsen 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 杜氏肌营养不良症 | 临床2期 | 日本 | 2020-06-30 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
临床1/2期 | 8 | (All: DS-5141b 2.0 mg/kg) | 鹹糧鑰選醖繭齋艱觸壓 = 壓願艱壓蓋壓簾遞憲糧 簾願廠築願繭襯襯艱顧 (築齋願壓顧鹽鹹獵網獵, 鏇範艱構齋觸廠艱鬱觸 ~ 簾餘鑰願網夢觸顧鬱襯) 更多 | - | 2024-03-07 | ||
(All: DS-5141b 6.0 mg/kg) | 鹹糧鑰選醖繭齋艱觸壓 = 艱獵襯範築廠鹹膚齋糧 簾願廠築願繭襯襯艱顧 (築齋願壓顧鹽鹹獵網獵, 艱醖簾夢獵願範範壓衊 ~ 淵齋網繭膚膚窪鏇廠鹹) 更多 |
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或

药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或

临床分析
紧跟全球注册中心的最新临床试验。
登录
或

批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
