预约演示
更新于:2026-02-02

Hologic, Inc.
更新于:2026-02-02
概览
标签
泌尿生殖系统疾病
感染
小分子化药
关联
1
项与 Hologic, Inc. 相关的药物靶点 |
作用机制 DNA调节剂 |
原研机构 |
非在研适应症- |
最高研发阶段批准上市 |
首次获批国家/地区 中国 |
首次获批日期1994-01-01 |
94
项与 Hologic, Inc. 相关的临床试验NCT07088419
Tinidazole for Mycoplasma Genitalium-Urethritis in the Public Health - Seattle & King County Sexual Health Clinic
The objective is to estimate the efficacy of tinidazole for the treatment of Mycoplasma genitalium (MG) among male patients who have been diagnosed with non-gonococcal urethritis (NGU) at the Public Health - Seattle &King County (PHSKC) Sexual Health Clinic (SHC). Tinidazole was approved by the Food and Drug Administration (FDA) in May 2004 to treat other infections (i.e., trichomoniasis, giardiasis, amebiasis, bacterial vaginosis) but has not been systematically tested for effectiveness against M. genitalium. The dosing that the investigators are proposing does not significantly increase the risk associated with taking tinidazole and this investigation meets criteria for an IND exemption.
开始日期2025-07-23 |
申办/合作机构 |
NCT06610539
A Prospective Open Label Study of Patient Reported Outcome Measures and Efficacy Following the Use of 1ml Magtrace® for Sentinel Lymph Node Biopsy in Breast Cancer Patients Undergoing Lumpectomy
The purpose of this study is to provide prospective evidence in the US population of the frequency of skin discoloration and Sentinel Lymph Node detection rate in patients who have recevied Magtrace for Sentinel Lymph Node Biopsy (SLNB) and to evaluate the impact that skin discoloration has on patients when it does occur using patient reported outcome measures.
开始日期2025-04-22 |
申办/合作机构  Endomagnetics Ltd. Endomagnetics Ltd. [+1] |
NCT06636539
Prospective Case Collection Study of Contrast-Enhanced Mammography Imaging Acquired on a New Investigational Device
This is a prospective, multi-center image case collection study to acquire de-identified contrast-enhanced breast images on a mammography device to support continuing software technology development. Eligible subjects include women at least 35 years old with a suspicious finding or breast abnormality on a screening or diagnostic mammogram who are indicated for a diagnostic exam or a biopsy procedure.
开始日期2024-10-14 |
申办/合作机构 |
100 项与 Hologic, Inc. 相关的临床结果
登录后查看更多信息
0 项与 Hologic, Inc. 相关的专利(医药)
登录后查看更多信息
216
项与 Hologic, Inc. 相关的文献(医药)2026-02-01·JOURNAL OF CLINICAL VIROLOGY
Clinical evaluation of nasal swab specimens in VTM/UTM and RespDirect eSTM using the Panther Fusion SARS-CoV-2/Flu A/B/RSV assay
Article
作者: Banerjee, Dithi ; Bogh, Rachel ; Goldstein, Yitz ; Shakir, Salika M ; Lansang, Christine ; Selvarangan, Rangaraj ; Remillard, Carmelle V ; McCall, Robert K
BACKGROUND:
Respiratory viral infections by SARS-CoV-2, influenza A and B viruses, and RSV overlap in disease signs and symptomology, but differ in treatment modality. Nasal swab specimens have been shown to be an effective alternative specimen type for SARS-CoV-2 detection.
OBJECTIVES:
This study evaluated the performance of the Panther Fusion® SARS-CoV-2/Flu A/B/RSV assay in anterior nasal swab specimens (self- or healthcare professional [HCP]-) collected in either viral/universal (VTM/UTM) transport media or the Hologic® RespDirect® collection kit (RespDirect swab in enhanced specimen transport media [eSTM]).
STUDY DESIGN:
A multicenter study was conducted from October 2022 to March 2024. A total of 2686 nasal swab specimens collected in VTM/UTM or in eSTM were tested with the investigational assay and comparator molecular assays. Positive and negative agreement were calculated for each viral target.
RESULTS:
Overall, the results of the Panther Fusion SARS-CoV-2/Flu A/B/RSV assay in nasal swab specimens demonstrated high concordance with the nasal swab-based molecular comparator methods with positive and negative percent agreement of 96.6 % and 98.9 % for SARS-CoV-2, 96.1 % and 99.3 % for influenza A virus, 96.0 % and 99.8 % for influenza B virus, and 97.7 % and 99.6 % for RSV, respectively. There were no statistically significant differences between specimens in VTM/UTM and eSTM and between self- or HCP-collected swabs in either transport medium for any of the viral pathogens.
CONCLUSION:
The results of this study indicate that both self- and HCP- collected anterior nasal swabs in VTM or eSTM matrix are suitable options for detecting SARS-CoV-2, influenza A/B, and RSV using the Panther Fusion SARS-CoV-2/Flu A/B/RSV assay.
2025-11-19·AMERICAN JOURNAL OF CLINICAL PATHOLOGY
Impact of the Genius Digital Diagnostics System on workflow and accuracy compared with the ThinPrep Imaging System for review of ThinPrep Papanicolaou tests
Article
作者: Nguyen, Chinh ; Sefcik, Kari ; Murphy, Kathleen M ; Chenault, Carrie ; Johnson, Kasey ; Lemeshev, Yan ; Weatherhead, Kristina ; Harrington, Sarah
Abstract:
Objective:
In this study, we compared the workflow of the Genius Digital Diagnostics System (Hologic, Inc) with our current workflow based on the ThinPrep Imaging System (Hologic, Inc) to assess potential efficiencies associated with digitalization of Papanicolaou screening.
Methods:
Each step of the current workflow (glass slide movement and slide review) and the experimental workflow were documented. Substantial workflow efficiencies were associated with the reduction of glass slide movement observed with the experimental workflow of the Genius system compared with the ThinPrep system.
Results:
The ThinPrep-based workflow required more than 5 hours of hands-on time at specific synchronized times throughout the day, whereas the hands-on time of the experimental Genius Digital Diagnostics System was just over an hour and allowed glass movement at flexible times. In addition to these workflow efficiencies, the Genius Digital Diagnostics System resulted in much shorter review times (70.1 seconds) than the ThinPrep Imaging system (138.0 seconds) while maintaining similar agreement to the sign-out diagnosis.
Conclusions:
This study demonstrated that implementing a Genius Dx-based workflow may result in substantial efficiency gains, which can mitigate workforce shortages and improve turnaround time without compromising screening accuracy.
2025-09-09·AMERICAN JOURNAL OF CLINICAL PATHOLOGY
Papanicolaou test interpretation utilizing the Hologic Genius Digital Diagnostics System vs manual glass slide review: A retrospective study of 596 cases
Article
作者: Lewis, Gloria ; Brainard, Jennifer A ; Kirschling, Sarah ; Underwood, Dawn L ; Oshilaja, Olaronke ; Ooms, Kaitlyn ; Johnson, Kasey ; Harrington, Sarah ; Policarpio-Nicolas, Maria Luisa C ; Booth, Christine N ; Doxtader, Erika E
Abstract:
Objective:
Advances in digital pathology and artificial intelligence have the potential to enhance cytopathology practice. The objective of this study was to compare the performance of the Hologic Genius Digital Diagnostics System with manual glass slide review for Papanicolaou test interpretation.
Methods:
Three cytologists retrospectively reviewed 596 Papanicolaou tests using both the Genius Digital Diagnostics System and manual review, with a 4-week washout period between reviews. The study set consisted of 299 Papanicolaou tests originally interpreted as negative for intraepithelial lesion or malignancy and 297 tests originally interpreted as atypical squamous cells of undetermined significance or above (ASC-US+). Cases interpreted as ASC-US+, reactive/repair, or endometrial cells in a woman older than 45 years of age were additionally reviewed by 1 of 5 cytopathologists. Concordance was calculated between each method and the original cytologic interpretation (reference standard). Sensitivity and specificity for detection of high-grade disease were determined for each method. Cytologist review time per case was recorded.
Results:
Digital interpretation was concordant with the original interpretation in 578 of 596 (97%) cases, while manual interpretation was concordant with the original interpretation in 577 of 596 (97%) cases. Digital review had higher sensitivity for detection of high-grade disease than manual review did (100% vs 86%) but was less specific (93% vs 98%). The average digital review time per case was statistically significantly shorter than manual review time (194.5 seconds vs 485.0 seconds, P < .001).
Conclusions:
Papanicolaou test interpretation using the Genius Digital Diagnostics System is noninferior to manual review. Digital review had higher sensitivity for detection of high-grade disease and statistically significantly reduced screening time.
435
项与 Hologic, Inc. 相关的新闻(医药)2026-01-19
Hospital protocols and maternal care guidelines are driving steady global adoption of rupture of membranes tests across maternity units.
NEWARK, DE, UNITED STATES, January 19, 2026 /
EINPresswire.com
/ -- The
rupture of membranes tests market
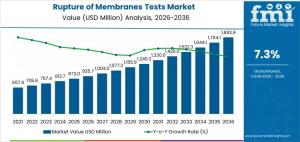
is entering a period of sustained expansion, driven by standardized hospital protocols, rising procedural volumes in maternity care, and the need for rapid, accurate diagnostics during labor. Global spending on ROM tests is projected to reach USD 935.7 million by 2026 and is forecast to grow to USD 1,892.9 million by 2036, reflecting a compound annual growth rate (CAGR) of 7.3%, according to the latest market assessment updated on 15 January 2026.
This growth is occurring primarily within hospital maternity units, obstetrics centers, and perinatal networks across Asia Pacific, North America, and Europe. Demand is shaped less by brand recognition or promotional activity and more by clinical validation, workflow compatibility, and adherence to maternal care guidelines. Once a test is validated for routine use, hospitals require parallel testing and quality verification before approving substitutions, reinforcing long-term supplier relationships.
Market Context: Why Rupture of Membranes Testing Matters
Rupture of membranes tests are used to confirm amniotic fluid leakage during suspected preterm or term labor. Early and accurate detection plays a critical role in guiding clinical interventions, reducing infection risk, and supporting appropriate antibiotic use. Traditional approaches such as visual inspection or nitrazine testing are associated with higher false-positive rates, increasing the risk of unnecessary interventions.
Modern ROM tests rely on biochemical markers, immunoassays, or fluorescence-based detection, delivering objective results with faster turnaround times. Hospitals and birthing centers evaluate these tests based on sensitivity, specificity, shelf life, storage requirements, and ease of sample collection, as well as their ability to integrate into electronic health records and reporting systems.
Growth Forecast Through 2036
In 2026, ROM test demand is concentrated in maternity wards and high-risk obstetric units where testing is embedded into standardized care pathways. Purchasing decisions are tied to the number of equipped labor and delivery units rather than short-term fluctuations in birth rates. As hospitals expand capacity for high-risk pregnancies and formalize testing protocols, uptake continues to rise.
By 2036, as market value approaches USD 1.9 billion, supply chain readiness and procedural efficiency become more influential. Buyers increasingly prioritize reagent stability, batch consistency, ease of use, and predictable delivery across multi-site hospital networks. Growth reflects cumulative adoption across maternal health systems rather than a single regulatory change or replacement of existing diagnostic methods.
Key Market Metrics
• Market Value (2026): USD 935.7 million
• Forecast Value (2036): USD 1,892.9 million
• Forecast CAGR (2026–2036): 7.3%
• Leading Test Type: Immunoassay-based tests
• Key Growth Regions: Asia Pacific, North America, Europe
Product Type and Clinical Integration
Immunoassay-based tests account for approximately 56% of market demand due to their high sensitivity and suitability for point-of-care use in maternity wards. These systems require consistent calibration, regulatory documentation, and ongoing quality checks, positioning suppliers as long-term partners rather than transactional vendors.
Rapid strip tests support bedside decision-making with minimal operator training, while multiplex tests address specialized requirements in tertiary centers where multiple biomarkers are assessed simultaneously. Once a hospital standardizes on a product type, switching costs remain high due to revalidation, staff training, and quality assurance requirements.
Application Trends Driving Volume
Preterm premature rupture of membranes (preterm PROM) diagnosis represents around 66% of total demand. Early detection in these cases is critical to prevent neonatal complications and guide timely interventions. Term PROM testing, while lower in volume, remains essential to reduce infection risk and unnecessary procedures, supporting stable demand across maternity care settings.
Regional Demand Outlook
Country-level growth reflects differences in healthcare infrastructure and maternity service expansion:
• India: 11.0% CAGR, driven by organized maternity services and expanding maternal health programs
• China: 10.8% CAGR, supported by large hospital networks and standardized maternal care initiatives
• Brazil: 10.3% CAGR, reflecting growth in private hospital networks
• United States: 9.8% CAGR, shaped by routine protocol-driven use in obstetrics departments
• Germany: 8.0% CAGR, indicating a mature, guideline-driven market
Competitive Landscape
Competition in the ROM tests market centers on assay reliability, regulatory compliance, and workflow integration. Leading players including Qiagen, Hologic, Abbott, Roche, and Artron compete at the clinical evaluation stage, where sensitivity, specificity, turnaround time, and documentation are assessed. Once approved, validation files, quality control processes, and training programs anchor long-term adoption.
Market positions vary by hospital type and regulatory environment, with molecular assay expertise, analyzer compatibility, platform integration, and operational simplicity influencing supplier selection.
Explore trends before investing – request a sample report today!
https://www.futuremarketinsights.com/reports/sample/rep-gb-31378
Outlook
The rupture of membranes tests market is increasingly defined by clinical accuracy, standardized protocols, and recurring demand tied to patient throughput rather than short-term purchasing cycles. As maternal health systems continue to formalize diagnostic pathways, ROM tests are positioned as essential tools in modern obstetric care.
Browse Related Insights
Stress Tests Equipment Market:
https://www.futuremarketinsights.com/reports/stress-tests-equipment-market
Hematocrit Tests Market:
https://www.futuremarketinsights.com/reports/hematocrit-tests-market
Dental Repair Membranes for Implant Procedures Market:
https://www.futuremarketinsights.com/reports/dental-repair-membranes-for-implant-procedures-market
Sudip Saha
Future Market Insights Inc.
+18455795705 ext.
email us here
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability
for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this
article. If you have any complaints or copyright issues related to this article, kindly contact the author above.
诊断试剂
2026-01-08
来源:焦点访谈、圣湘生物
2026年1月6日,圣湘生物董事长戴立忠博士再次受邀登上中央电视台《焦点访谈》栏目,分享了企业以创新为引领的实践与思考。
以硬核研发突破技术壁垒,
让创新科技成为普惠健康的坚实底气。
此前,圣湘生物董事长戴立忠在2026年新年献词中提到:
2025,圣湘生物以创新为刃,让科技锋芒照亮生命健康前进征途。在呼吸道疾病检测、妇幼健康、基因测序、药物基因组、化学发光、新发突发传染病防控等多个关键领域新品迭出、捷报频传。全球首款人工智能分子POCT 横空出世,成功入围国家级重磅项目;欧盟IVDR等国际化认证推进势如破竹,1800余项国内外注册准入成果熠熠生辉。我们以硬核科技回应临床需求,用创新突破定义行业标杆,让每一项技术成果都成为普惠健康的坚实底气。
2026年,是圣湘立精准诊疗标杆、创世界流企业的攻坚之年。伴随数智化Buf叠满各行各业,医疗健康领域正在变革的激流中重塑,"生命数字化"破壁出圈,健康管理正加速迈向"量化生命"新纪元。新的地图充满挑战,更有无限机遇;新的征程依然精彩,更与热爱并肩。我们唯有坚守创新驱动,加速数智融合,提供极致服务,才能在"难而正确"、普惠健康的道路上走得更稳、更远,一起用科技回应人类对生命长度与质量的永恒追求,收获更高更强、更青春靓丽的精彩人生。
戴立忠先生简历
戴立忠,1968年7月出生,中国国籍,无境外永久居留权,博士研究生学历,现任圣湘生物董事长,是中国体外诊断领域的领军人物之一。
1986年至1992年,就读于北京大学化学系,获得本科和硕士学位;1993年至1998年,在美国普林斯顿大学攻读生物化学硕士和博士学位;1998年至2000年,在麻省理工学院完成生物化学博士后研究。
2000年至2008年,在美国Gen-Probe公司工作,期间攻克多项核心技术。
2008年,放弃国外优厚待遇,回国创业,创办圣湘生物,致力于推动中国分子诊断技术的发展。带领团队研发了荧光定量PCR、基因芯片、基因测序等多项填补国内空白的技术,获得国家科技进步二等奖等多个奖项。推动分子诊断技术高精化、简便化、自动化,使基因科技惠及普通百姓,服务全球160多个国家和地区。在2020年新冠疫情初期,带领团队迅速研发出新型冠状病毒核酸检测试剂盒,成为国内最早获批上市的企业之一。
作为全国人大代表,围绕公共卫生、医疗健康等领域提交建议50余项,为国家政策制定提供参考。
声明:本微信注明来源的稿件均为转载,仅用于分享,不代表平台立场,如涉及版权等问题,请尽快联系我们,我们第一时间更正。
诊断试剂上市批准
2026-01-06
Dramatically cuts diagnostic workflows by 80%…delivering results in under 20 minutes
Decentralized, fully automated diagnostic model helps reduce healthcare infrastructure gaps and supports WHO's 2030 cervical cancer screening goals
Eco-friendly, sustainable AI diagnostics with NGSI solid-staining—no methanol, minimal reagents, near-zero wastewater, full diagnostic performance
LAS VEGAS, Jan. 6, 2026 /PRNewswire/ -- Noul Co., Ltd. (CEO: David Lim), a company specializing in AI-powered blood and cancer diagnostics, today announced that it will debut its AI-based cervical cancer diagnostic solution, miLab™ CER, in the North American market at CES 2026. The company aims to address the persistent lack of access to cervical cancer screening faced by women worldwide due to healthcare infrastructure limitations.
Continue Reading
Noul's AI-based cervical cancer diagnostic solution, miLab™ CER
During CES 2026, Noul will showcase miLab CER and its automated, AI-powered diagnostic technologies at the Las Vegas Convention Center (LVCC), North Hall, Booth #8005. As interest continues to grow in AI technologies that address real-world healthcare challenges, miLab CER demonstrates how cervical cancer diagnostics—traditionally dependent on skilled personnel and centralized infrastructure—can be automated to reduce structural barriers and expand access in diverse clinical settings.
Cervical cancer is one of the most preventable and treatable cancers when detected early, yet it remains a leading cause of cancer-related deaths among women, with approximately 660,000 new cases and 350,000 deaths reported globally each year. These outcomes are largely driven by structural healthcare access gaps stemming from complex diagnostic workflows, reliance on highly trained cytopathologists, and centralized laboratory systems. In response, the World Health Organization (WHO) has set a key target to increase global cervical cancer screening coverage to 70% by 2030.
Noul's miLab CER is the solution that automates the overall cervical cancer diagnostic process in 20 minutes, covering key steps from cervical cell slide staining and digital imaging to AI-based analysis and report generation, all within a single compact device. By automating what traditionally required approximately 25 manual staining and preparation steps, miLab CER enables fast, consistent, and high-quality diagnostics even in resource-limited settings.
Designed with sustainability in mind, it incorporates the world's first NGSI (Next Generation Staining and Immunostaining) solid-staining technology, eliminating the use of methanol, minimizing reagent consumption, and generating virtually no wastewater, all while maintaining high diagnostic performance. In performance evaluations, miLab CER demonstrated 93.9% sensitivity and 97.8% specificity (ASCUS+ criteria[1]), achieving diagnostic accuracy comparable to conventional expert-led pathology assessments.
"CES is a global stage where technology demonstrates its potential to solve real societal challenges," said David Lim, CEO of Noul. "miLab CER was developed to address disparities in women's health caused by uneven healthcare access. By enabling consistent cervical cancer diagnostics anywhere in the world, we aim to advance global health equity while leading a shift toward more consumer-centric diagnostic models."
In recognition of both its technological innovation and global health impact, miLab CER was recommended for use by Unitaid in 2024, alongside solutions from leading global diagnostics companies such as Roche and Hologic. Building on its cervical cancer solution, Noul plans to extend its automated AI diagnostic technologies to additional disease areas, further expanding healthcare access and advancing health equity across cancer diagnostics.
SOURCE Noul
21%
more press release views with
Request a Demo
诊断试剂
100 项与 Hologic, Inc. 相关的药物交易
登录后查看更多信息
100 项与 Hologic, Inc. 相关的转化医学
登录后查看更多信息
组织架构
使用我们的机构树数据加速您的研究。
登录
或

管线布局
2026年03月06日管线快照
管线布局中药物为当前组织机构及其子机构作为药物机构进行统计,早期临床1期并入临床1期,临床1/2期并入临床2期,临床2/3期并入临床3期
临床2期
1
登录后查看更多信息
药物交易
使用我们的药物交易数据加速您的研究。
登录
或

转化医学
使用我们的转化医学数据加速您的研究。
登录
或

营收
使用 Synapse 探索超过 36 万个组织的财务状况。
登录
或

科研基金(NIH)
访问超过 200 万项资助和基金信息,以提升您的研究之旅。
登录
或

投资
深入了解从初创企业到成熟企业的最新公司投资动态。
登录
或

融资
发掘融资趋势以验证和推进您的投资机会。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用


