预约演示
更新于:2026-02-27
Tominersen
更新于:2026-02-27
概要
基本信息
非在研机构 |
最高研发阶段临床2期 |
首次获批日期- |
最高研发阶段(中国)终止 |
特殊审评孤儿药 (美国) |
登录后查看时间轴
结构/序列
使用我们的RNA技术数据为新药研发加速。
登录
或
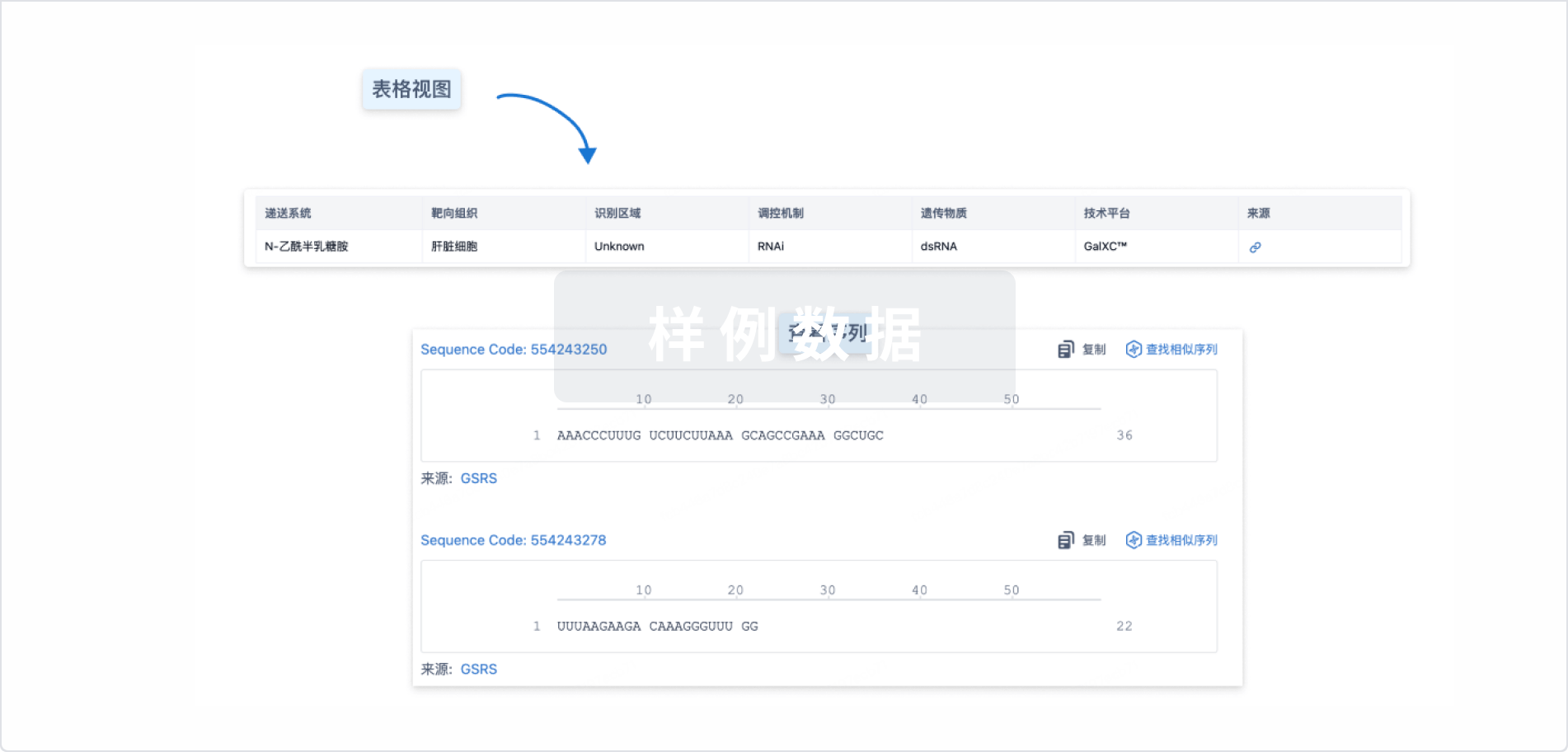
Sequence Code 317419970

来源: *****
关联
6
项与 Tominersen 相关的临床试验NCT05686551
A Phase II, Randomized, Double-blind, Placebo-controlled, Dose-finding Study to Evaluate the Safety, Biomarkers, and Efficacy of Tominersen in Individuals With Prodromal and Early Manifest Huntington's Disease
This study will evaluate the safety, biomarkers, and efficacy of tominersen compared with placebo in participants with prodromal and early manifest Huntington's Disease (HD).
开始日期2023-02-03 |
申办/合作机构 |
NCT04000594
An Open-Label Adaptive Multiple-Dose Study to Investigate the Pharmacokinetics and Pharmacodynamics of RO7234292 in CSF and Plasma, and Safety and Tolerability Following Intrathecal Administration in Patients With Huntington's Disease
Study BP40410 is an open-label, adaptive multiple-dose clinical study designed to characterize the PK of RO7234292 (RG6042) in plasma and CSF as well as the acute time course and recovery profile of CSF mHTT lowering in response to RO7234292 (RG6042) treatment after intrathecal (IT) administration of RO7234292 (RG6042) to patients with manifest Hungtington's disease (HD).
开始日期2019-09-02 |
申办/合作机构 |
NCT03842969
An Open-Label Extension Study to Evaluate the Long-Term Safety and Tolerability of Intrathecally Administered RO7234292 (RG6042) in Patients With Huntington's Disease
This study will evaluate the long-term safety and tolerability of RO7234292 (RG6042) in participants who have completed other F. Hoffmann-La Roche, Ltd.-sponsored and/or Genentech-sponsored studies in the Huntington's disease (HD) in the development program for RG6042.
开始日期2019-04-23 |
申办/合作机构 |
100 项与 Tominersen 相关的临床结果
登录后查看更多信息
100 项与 Tominersen 相关的转化医学
登录后查看更多信息
100 项与 Tominersen 相关的专利(医药)
登录后查看更多信息
13
项与 Tominersen 相关的文献(医药)2025-12-01·Molecular Therapy-Nucleic Acids
Molecular and imaging biomarker responses to brain mutant HTT lowering in a mouse model of Huntington disease
Article
作者: Bale, Kirsten ; Anderson, Christine ; Fan, Jianjia ; Ko, Seunghyun ; Wellington, Cheryl L ; Yung, Andrew ; Hayden, Michael R ; Kozlowski, Piotr ; Pouladi, Mahmoud A ; Caron, Nicholas S ; Ma, Da
Therapies targeting mutant huntingtin (mHTT) reduction in the brain hold promise as disease-modifying treatments for Huntington disease (HD), necessitating biomarkers that accurately reflect treatment response. We evaluated candidate molecular and imaging biomarkers after mHTT reduction in YAC128 HD mice, with equal numbers of males and females per group. At 6 months of age, YAC128 mice received unilateral intracerebroventricular injections of saline or mHTT-lowering antisense oligonucleotide (HTT ASO). Plasma neurofilament light chain (NEFL) and glial fibrillary acidic protein (GFAP) were measured longitudinally from 6 to 12 months. Structural MRI was performed at 6, 9, and 12 months. At study endpoint, we quantified mHTT target engagement in the brain and performed striatal RNA sequencing. Treatment with HTT ASO produced a sustained reduction of mHTT levels throughout the brain for up to 6 months, significantly slowed plasma NEFL increases, and moderately attenuated GFAP elevation. Although mHTT levels inversely correlated with gray and white matter volumes, treatment did not significantly stabilize regional brain atrophy, highlighting an association between mHTT load and neuroanatomical integrity. HTT ASO also partially reversed striatal transcriptome dysregulation and restored oligodendrocyte-specific gene expression. Plasma NEFL, but not brain imaging, emerges as a sensitive and dynamic response biomarker for mHTT-lowering therapies.
2024-09-01·Molecular Therapy-Nucleic Acids
Preclinical evaluation of stereopure antisense oligonucleotides for allele-selective lowering of mutant HTT
Article
作者: Prakasha, Priyanka Shiva ; Taborn, Kristin ; Francis, Christopher ; Byrne, Mike ; Kandasamy, Pachamuthu ; Frank-Kamenetsky, Maria ; Upadhyay, Hansini ; Maguire, Abbie ; Jang, Hyun Gyung ; Purcell-Estabrook, Erin ; Yang, Hailin ; Dale, Elena ; Iwamoto, Naoki ; Meena ; Shimizu, Mamoru ; Hu, Xiao Shelley ; Shelke, Juili Dilip ; Yin, Yuan ; Tseng, Wei Chou ; Zhao, Anderson ; Liu, Yuanjing ; Longo, Ken ; Akhtar, Ali ; Metterville, Jake ; Verdine, Gregory L ; Looby, Richard ; Liu, Fangjun ; Kothari, Nayantara ; Lamattina, Anthony ; Pan, Qianli ; Bowman, Keith ; Standley, Stephany ; Vargeese, Chandra
Huntington's disease (HD) is an autosomal dominant disease caused by the expansion of cytosine-adenine-guanine (CAG) repeats in one copy of the HTT gene (mutant HTT, mHTT). The unaffected HTT gene encodes wild-type HTT (wtHTT) protein, which supports processes important for the health and function of the central nervous system. Selective lowering of mHTT for the treatment of HD may provide a benefit over nonselective HTT-lowering approaches, as it aims to preserve the beneficial activities of wtHTT. Targeting a heterozygous single-nucleotide polymorphism (SNP) where the targeted variant is on the mHTT gene is one strategy for achieving allele-selective activity. Herein, we investigated whether stereopure phosphorothioate (PS)- and phosphoryl guanidine (PN)-containing oligonucleotides can direct allele-selective mHTT lowering by targeting rs362273 (SNP3). We demonstrate that our SNP3-targeting molecules are potent, durable, and selective for mHTT in vitro and in vivo in mouse models. Through comparisons with a surrogate for the nonselective investigational compound tominersen, we also demonstrate that allele-selective molecules display equivalent potency toward mHTT with improved durability while sparing wtHTT. Our preclinical findings support the advancement of WVE-003, an investigational allele-selective compound currently in clinical testing (NCT05032196) for the treatment of patients with HD.
2024-08-01·Current Neurology and Neuroscience Reports
Huntington’s Disease: Latest Frontiers in Therapeutics
Review
作者: Mestre, Tiago A ; Saade, Joseph
PURPOSE OF REVIEW:
Huntington's disease (HD) is an autosomal-dominant disorder caused by a pathological expansion of a trinucleotide repeat (CAG) on exon 1 of the huntingtin (HTT) gene. HD is characterized by the presence of chorea, alongside other hyperkinesia, parkinsonism and a combination of cognitive and behavioural features. Currently, there are no disease-modifying therapies (DMTs) for HD, and the only intervention(s) with approved indication target the treatment of chorea. This article reviews recent research on the clinical development of DMTs and newly developed tools that enhance clinical trial design towards a successful DMT in the future.
RECENT FINDINGS:
HD is living in an era of target-specific drug development with emphasis on the mechanisms related to mutant Huntingtin (HTT) protein. Examples include antisense oligonucleotides (ASO), splicing modifiers and microRNA molecules that aim to reduce the levels of mutant HTT protein. After initial negative results with ASO molecules Tominersen and WVE-120101/ WVE-120102, the therapeutic landscape continues to expand, with various trials currently under development to document proof-of-concept and safety/tolerability. Immune-targeted therapies have also been evaluated in early-phase clinical trials, with promising preliminary findings. The possibility of quantifying mHTT in CSF, along with the development of an integrated biological staging system in HD are important innovations applicable to clinical trial design that enhance the drug development process. Although a future in HD with DMTs remains a hope for those living with HD, care partners and care providers, the therapeutic landscape is promising, with various drug development programs underway following a targeted approach supported by disease-specific biomarkers and staging frameworks.
64
项与 Tominersen 相关的新闻(医药)2026-01-06
iStock,
Grandfailure
Recent breakthroughs and three decades of progress in treating Huntington’s disease
The past 10 years have seen landmark moments for several neurodegenerative conditions. From the 2023 approvals of disease-modifying therapies for
Alzheimer’s
and a subtype of
amyotrophic lateral sclerosis
(ALS) to
uniQure’s data
in September showing that its gene therapy slowed progression in Huntington’s by 75%, the sector has seemingly begun to break through in these intractable diseases.
Families with Huntington’s need this to be true more than most. The devastating neurodegenerative disease is caused by a CAG repeat in the first exon of the huntingtin (HTT) gene. While this gene was first discovered in 1993, the ensuing 32 years have seen a trickle of incremental progress, with only symptomatic treatments emerging as candidates by Roche, Wave Life Sciences, Sage Therapeutics and more failed to effectively conquer the disease itself.
September’s
readout
by uniQure sparked new hope for the approximately
41,000 Americans
living with Huntington’s—and over 200,000 more who carry the genetic mutation. While uniQure was full speed ahead with plans to submit a biologics license application early next year, the FDA has seemingly reversed position on the therapy. Feedback from a
pre-BLA meeting
revealed by the company in December indicated the agency “no longer agrees” that data from its Phase I/II trials would be “adequate to provide the primary evidence in support of a BLA submission.”
However, the Dutch biotech is hardly alone in a Huntington’s market that is projected to reach
nearly $1.9 billion by 2030
.
Resilient Pipeline
After Roche and Ionis
stopped
a Phase III trial in 2021 for their antisense oligonucleotide (ASO)
tominersen
, Roche revitalized the asset based on a
post-hoc analysis
showing that low-exposure of the drug may benefit younger adult patients with lower disease burden. Tominersen is now being investigated in a
Phase II clinical trial
for patients with prodromal and early manifest Huntington’s. That trial is expected to be completed in spring 2027.
2021 was also a bad year for Wave, which
shelved two ASO therapies
a week after Roche’s unfortunate news. But Wave is back too, with a next-generation ASO called WVE-003 that the company plans to take into a Phase II/III trial this quarter. The Cambridge, Mass.–based biotech has also aligned with the FDA on a path to accelerated approval, using the slowing of caudate atrophy—which has been strongly linked to a reduction in mutant huntingtin protein—as a clinical surrogate endpoint.
Editor’s note: A version of this article was originally published as a special edition of
ClinicaSpace
on Nov. 3, 2025.
.responsive-container {
display: flex;
flex-wrap: wrap;
border: 1px solid #ededed;
font-family: Helvetica, Arial, Sans-Serif;
padding: 20px 20px 10px 20px;
}
.column-left {
flex: 1;
max-width: 45%;
padding: 20px 20px 10px 20px;
}
.column-right {
flex: 2;
padding: 20px 20px 10px 20px;
}
@media (max-width: 768px) {
.column-left,
.column-right {
max-width: 100%;
flex: 100%;
padding: 10px 0;
}
}
Subscribe to ClinicaSpace!
Clinical trial results, research news, the latest in cancer, cell and gene therapy
hbspt.forms.create({
region: "na1",
portalId: "4413123",
formId: "674f4dc0-7371-4190-86cc-e1afd00b08ea",
onFormSubmitted: function($form, data) {
window.dataLayer = window.dataLayer || [];
window.dataLayer.push({
'event': 'GTMevent',
'event_name': 'newsletter_sign_up'
});
}
});
临床2期基因疗法临床3期寡核苷酸
2025-12-23
·知乎专栏
原文出处:Big生物创新社;老狼略有删改原文链接:2025年对于生物制药行业来说仍然是充满挑战但又不乏曙光的一年。面对盈利目标落空、融资成本飙升和监管不确定性加剧带来的重重困难,药企管线的含金量仍在持续上升,各新型疗法进入收获期,凭借对颠覆性技术的持续探索,各家药企仍在致力将创新疗法更好更快地推向市场。本文将回顾今年最具意义的5项临床试验关键进展,探讨其对公司和行业的广泛影响。01 uniQure亨廷顿病疗法疾病延缓75%,30余年无药困局迎希望亨廷顿病(Huntington's Disease,HD)是一种致命的常染色体显性遗传性神经退行性疾病,由HTT基因第1号外显子CAG重复序列异常扩增引起,导致突变亨廷顿蛋白(mHTT)毒性累积。患者通常在30-50岁发病,表现为不自主舞蹈样运动、认知衰退和精神症状,病程10-25年,最终因吞咽困难、肺部感染或心衰离世。目前无药可医,现有药物只能部分缓解运动症状,无法延缓或逆转疾病进程。目前市面上仅有丁苯那嗪及其升级版氘丁苯那嗪两款症状缓解药物,治标不治本。此前,罗氏和lonis合作开发的反义寡核苷酸(ASO)疗法tominersen曾一度被寄予厚望,但因疗效不佳,其Ⅲ期临床试验GENERATION HD1于今年3月终止。当下市场主要关注的是uniQure的AMT-130和Wave Life Sciences的WVE-003(PNASO),而后者2024年公布的1期数据显示,多剂量给药下,24周后和28周后mHTT分别平均降低46%和44%。9月24日,uniQure公布了其AAV5递送的miRNA基因疗法AMT-130用于早期HD的1/Ⅱ期临床试验的长期随访结果。数据显示,其在安全性、关键生物标志物及多项临床评估指标上均表现出色,高剂量治疗效果可持续至治疗后三年,疾病进展显著减缓75%,以远超预期的数据结果达到主要终点,与此前公布的两年随访数据中的80%疾病进展减缓率也基本一致。此外,该药物还达到了关键的次要终点,经衡量生活自理能力的总功能能力(TFC)评估,与对照组相比,疾病进展显著减缓60%。其他临床指标上也呈现出有利趋势,整体耐受性良好,安全性特征可控。AMT-130基于uniQure 专利miQURE基因沉默技术开发,采用AAV5为载体,将靶向亨廷顿基因的人工micro-RNA送至脑组织,通过抑制mHTT产生,实现对疾病根源的精准干预。该药预计于2026年提交BLA,若能顺利获批,则有望成为全球首个针对HD治疗的基因疗法。但挑战仍存。首先是商业化压力,复杂的生产和递送工艺可能导致高昂的治疗成本,参照其他基因疗法、价格或成为AMT-130普及的障碍。其次是FDA的态度转变,uniQure本月再次表示,目前的Ⅰ/Ⅱ研究数据不太可能作为BLA申请的主要证据。公司正在仔细评估反馈意见,并计划紧急请求在2026年Q1与FDA举行后续会议。02 Metsera GLP-1减重药部分数据超替尔泊肽,引MNC竞购的减重新星2024年9月,聚焦肥胖症治疗的新兴选手Metsera宣布,其GLP-1注剂MET-097i在一项早期研究中于36天内实现了7.5%的减重效果,迅速引起了业界关注。今年,这家生物技术公司用实际行动证明了其成功并非偶然,并最终以近100亿美元的价格被收购。传统GLP-1药物同时激活G蛋白和β-arrestin通路,可能引发副作用,而MET-097i则是一款采用偏向型激活机制的GLP-1受体激动剂,通过选择性激活G蛋白通路,提升疗效的同时规避脱敏问题,实现更优的疗效-安全性平衡。给药频率方面,该药的优势也十分明显。相较于需每周注射一次的诺和诺德的Wegovy和礼来的Zepbound、Mounaro,MET-097i仅需每月注射一次。今年1月,Metsera公布了其la期临床试验数据。该试验纳入了120名超重或肥胖但未患2型糖尿病的患者,数据显示,经过12周的每周一次注射后,接受GLP-1注射的患者体重较安慰剂组下降了11.3%,且在12mg剂量组中个体反应高达约20%,并且没有观察到任何平台期效应。9月下旬,该司又发布了一项llb试验的数据,称1.2mg剂量组患者在28周时,安慰剂校正的平均体重减轻幅度高达14.1%。分析师指出,在类似随访期内,礼来的重磅药物替尔泊肽“安慰剂校正后体重减轻约为13%”。此外,该试验中,MET-097i个体最大减重幅度可达26.5%。研究延长期每周给药阶段(36周)结束时的探索性分析进一步显示,患者仍在显著减重,且尚未达到平台期。此外,Metsera公司的超长效胰淀素注剂MET-233i也值得一提。6月公布的一项Ⅰ期临床试验数据显示,与安慰剂组相比,36天后接受MET-233i治疗的受试者体重减轻了8.4%,个别受试者的体重减轻幅度甚至达到10.2%。Metsera正加速推进MET-233i的相关研究,包括单药疗法以及与MET-097i的联合疗法。9月中旬,辉瑞宣布将以企业价值49亿美元(每股47.50美元现金)收购Metsera,外加最高24亿美元的里程碑付款,潜在总对价达73亿美元。几项资产进展惨淡后,辉瑞此举竟在扩充其肥胖症领域管线,以此在潜力巨大的减重市场分一杯羹——辉瑞目前没有注射型减肥药,而口服药方面,由于肝脏安全问题,已先后停止了两种口服GLP-1候选药物lotiglipron和danuglipron的研发。一个月后,诺和诺德半路杀出,提出企业价值60亿美元(每股56.50美元)、最高90亿美元的竞购报价。而Metsera笑纳竞价的态度更是加剧了这场混战。辉瑞迅速反击,一方面提升报价,另一方面发起诉讼,指控诺和诺德“滥用市场主导地位”,“绕过反垄断法”以“压制竞争”。这场拉锯战以辉瑞胜诉收场,最终报价企业价值70亿美元(每股65.60美元)叠加新的里程碑付款(最高每股20.65美元),以总价值约100亿的方案完成了对M的收购。03 诺和诺德GLP-1/AmylinⅡ期数据亮眼,新一代减重药蓄势待发尽管诺和诺德竞购失利,其口服胰淀素候选药物Amycretin的期数据仍以“竞争性”疗效助其在减重降糖领域赢回一局。Amycretin是诺和诺德自主研发的一款新型长效共激动剂,能够同时激活GLP-1受体和胰注素(Amylin)受体。这种双重作用机制使其在减重和血糖控制方面具有显著潜力。今年年初,诺和诺德公布其针对超重/肥胖症患者的Ⅰ/Ⅱa期试验数据,结果显示,36周后,服用20mg剂量的Amycretin组受试者体重降幅达22%(vs. 安慰剂组2%)。上月,该司公布该产品首次用于2型糖尿病的Ⅱ期试验结果。该试验旨在评估在448名二甲双胍联用或不联用SGLT2抑制剂作为标准治疗血糖控制不佳的2型糖尿病患者中,使用每周一次皮下注射或每日一次口服Amycretin的安全性和疗效。数据显示,36周后,皮下注射m组体重降幅达14.5%(vs. 安慰剂组2.6%),口服Amycretin治疗组患者则实现了10.1%的降幅(vs. 安慰剂组2.5%),而无论哪种给药方式,高剂量Amycretin治疗在36周时均未观察到达到减重平台期。同时,Amycretin还能降低血糖水平(以糖化血红蛋白HbA1c表示),皮下注射组和口服组的最大降幅分别为1.8%和1.5%。AmycretinⅡ期临床试验的成功,对诺和诺德的肥胖症管线来说无疑是一剂强心针。近来这家公司在临床和商业上双双遇冷。尽管重磅药物Wegow率先上市,但其市场份额却不断被礼来的Zepbound蚕食。去年12月,其新一代减重疗法CagniSema虽然在期REDEFINE1研究中达到了主要终点,但22.7%的减重效果远低于投资者预期,导致该公司市值蒸发约720亿美元。与此同时,在期EVOKE和EVOKE+研究中,司美格鲁肽未能显著延缓阿尔茨海默病的进展。尽管此前大家对该项目的预期并不高,但数据公布后,诺和诺德的股价仍旧下跌了约10%。可以预见的是,这款产品将成为诺和诺德进展最快的高潜竞品,为进一步增长带来极大信心。目前,诺和诺德计划于2026年Q1启动皮下注射和口服Amycretin针对超重或肥胖成年人的Ⅲ期试验。此外,后续其还将推动GLP-1/GIP/GGG(联邦制药引进)、两款GLP-1/GIP/Amylin三靶点激动剂的临床开发,以进一步增强管线矩阵。04 BMS/BioNTech PD-1/VEGF药物验证地域一致性疗效,瞄准双抗布局领先PD-1/VEGF在当今癌症领域可谓最受关注的趋势之一。该疗法利用双特异性抗体结合并阻断两种受体,以独特的协同机制,迅速成为全球药企争相布局之选。去年9月,康方生物和Summit Therapeutics合作研发的依沃西单抗凭借显著的无进展生存期(PFS)获益,在针对晚期非小细胞肺癌(NSCLC)的头对头试验中战胜K药,让这一疗法一时更加声名大噪。几个月后,BioNTech也加速进军这一领域。在此前战略合作的基础上,以高达9.5亿美元的价格直接收购了普米斯,从而完全拥有获得这家中国biotech的PD-1/VEGF双抗BNT327。这款药物由人源化的抗PD-L1单域抗体(VHH)与一个含有Fc-沉默突变的抗VEGF-A IgG1抗体融合而成,能够通过结合PD-L1恢复效应T细胞功能,同时中和肿瘤微环境中的VEGF-A。通过同时作用于这两个靶点,可以从多个角度对肿瘤进行抑制,一方面调节肿瘤免疫微环境,另一方面影响肿瘤的血管生成,从而实现更好的治疗效果,并有助于提高安全性。这笔投资给BioNTech带来了丰厚回报。今年6月,BMS向BioNTech抛出橄榄枝,豪掷111亿美元获得该药的全球合作开发和商业化权利。临床方面,9月,该司公布了一项全球Ⅱ期临床试验的数据,结果显示, pumitamig(BNT327)与标准化疗联合使用,在广泛期小细胞肺癌(ES-SCLC)患者中取得了76.3%的确认客观缓解率(cORR),疾病控制率(DCR)则达到了100%,与此前在2025年欧洲肺癌大会(ELCC)上公布的在中国开展的Ⅱ期临床试验数据整体一致,现已获FDA治疗SCLC的孤儿药认定。本月,其针对晚期三阴性乳腺癌(TNBC)治疗的全球期临床试验结果也已公布。数据显示,无论PD-L1表达水平如何,pumitamig联合化疗均取得了不俗疗效,cORR为61.5%,DCR达92.3%,同样证实了之前在中国开展一线TNBC Ⅰb/Ⅱ期临床试验时观察到的治疗效果。目前,BioNTech已将pumitamig推进至同一适应症的后期研发阶段,并开展了期临床试验ROSETTA-LUNG-01。为了验证其在不同患者群体中的疗效,该研究正在美国、英国、土耳其、中国、韩国和澳大利亚等多个地区招募患者,并计划在全球范围内开设更多试验中心。ROSETTA-LUNG-01预计将于2029年3月完成。05 罗氏阿尔茨海默病疗法失败抗体获新生,临床进展助力重振旗鼓在神经科学领域研究进展受挫是常事,2025年也不例外。许多公司在这一领域遭遇临床试验失败,而罗氏今年却在最棘手的适应症之一阿尔茨海默病(AD)上取得了关键胜利在AD治疗中,能够减缓神经退化的治疗方法相对较少。β-淀粉样蛋白(Aβ)是AD的关键病理特征之一,Aβ会异常聚集形成淀粉样蛋白斑块,干扰神经细胞之间的信号传递,导致神经细胞功能障碍和死亡。取得进展的关键之一在于提高穿越血脑屏障(BBB)、进入中枢神经系统的能力,进而实现Aβ斑块的清除。2022年底,罗氏的Aβ抗体gantenerumab在两项Ⅲ期临床试验中均告失败,项目被迫终止。然而,通过采用其创新的脑穿梭药物递送技术“Brainshuttle”,罗氏以2+1的设计方式推出trontinemab,将gantenerumab与靶向转铁蛋白受体1(TfR1)的蛋白域融合在一起,利用脑血管内皮细胞上高表达的TfR1,通过受体介导的转胞吞(transcytosis)跨越血脑屏障,将更多的gantenerumab成功递送到中枢神经系统中,并在中枢通过抗体依赖的胞吞作用(ADCP)清除聚集的Aβ斑块。这种Brainshuttle技术使得trontinemab在低剂量下就能在中枢神经系统中实现高暴露量,从而更有效地清除大脑中的Aβ斑块,同时降低了因高剂量给药而带来的副作用风险。从2023年的阿尔茨海默病临床试验会议(CTAD)开始,罗氏就陆陆续续公布出了trontinemab临床Ⅰ期爬坡的临床数据,引起不少关注。今年7月,该司在2025年阿尔茨海默病协会国际会议(AAIC)上公布了Ⅰb/Ⅱa Brainshuttle AD试验结果。数据显示,治疗7个月内,91%接受高剂量trontinemab(3.6mg/kg)治疗的患者在PET扫描中脑部淀粉样蛋白检测呈阴性,其中72%实现了淀粉样蛋白团块的“深度清除”,且副作用情况较现有抗淀粉样蛋白治疗更少、更轻。在本月初举行的2025 CTAD上,罗氏也再次报告了这种更低剂量、更少副作用、更精准进入大脑的临床表现。基于整体结果,罗氏已正式启动两个平行的 III 期研究(TRONTIER 1 & 2),以进一步验证其在早期阿尔茨海默病人群中的疗效与安全性。Trontinemab的早期数据不仅标志着罗氏逆转了AD领域的失败阴影,也意味着AD治疗四十余年的研究终于有望迎来关键成果。期待其Ⅲ期试验后续进展,为AD治疗带来切实有效的新选择。结语 2025年,生物制药行业在重重挑战中砥砺前行,却也收获了令人瞩目的关键临床突破,相信未来将会有更多创新疗法涌现,为患者带来更多的治疗选择和希望,助力全球医疗水平迈向新的高度。引用各药企官网新闻、会议公开资料
基因疗法临床1期寡核苷酸
2025-12-19
作者|与安
2025年对于生物制药行业来说仍然是充满挑战但又不乏曙光的一年。面对盈利目标落空、融资成本飙升和监管不确定性加剧带来的重重困难,药企管线的含金量仍在持续上升,各新型疗法进入收获期,凭借对颠覆性技术的持续探索,各家药企仍在致力将创新疗法更好更快地推向市场。
本文将回顾今年最具意义的5项临床试验关键进展,探讨其对公司和行业的广泛影响。
01
uniQure亨廷顿病疗法:
疾病延缓75%,30余年无药困局迎希望
亨廷顿病(Huntington's Disease,HD)是一种致命的常染色体显性遗传性神经退行性疾病,由HTT基因第1号外显子CAG重复序列异常扩增引起,导致突变亨廷顿蛋白(mHTT)毒性累积。患者通常在30-50岁发病,表现为不自主舞蹈样运动、认知衰退和精神症状,病程10-25年,最终因吞咽困难、肺部感染或心衰离世。目前无药可医,现有药物只能部分缓解运动症状,无法延缓或逆转疾病进程。
目前市面上仅有丁苯那嗪及其升级版氘丁苯那嗪两款症状缓解药物,治标不治本。此前,罗氏和lonis合作开发的反义寡核苷酸(ASO)疗法tominersen曾一度被寄予厚望,但因疗效不佳,其Ⅲ期临床试验GENERATION HD1于今年3月终止。当下市场主要关注的是uniQure的AMT-130和Wave Life Sciences的WVE-003(PNASO),而后者2024年公布的1期数据显示,多剂量给药下,24周后和28周后mHTT分别平均降低46%和44%。
9月24日,uniQure公布了其AAV5递送的miRNA基因疗法AMT-130用于早期HD的1/Ⅱ期临床试验的长期随访结果。数据显示,其在安全性、关键生物标志物及多项临床评估指标上均表现出色,高剂量治疗效果可持续至治疗后三年,疾病进展显著减缓75%,以远超预期的数据结果达到主要终点,与此前公布的两年随访数据中的80%疾病进展减缓率也基本一致。此外,该药物还达到了关键的次要终点,经衡量生活自理能力的总功能能力(TFC)评估,与对照组相比,疾病进展显著减缓60%。其他临床指标上也呈现出有利趋势,整体耐受性良好,安全性特征可控。
AMT-130基于uniQure 专利miQURE基因沉默技术开发,采用AAV5为载体,将靶向亨廷顿基因的人工micro-RNA送至脑组织,通过抑制mHTT产生,实现对疾病根源的精准干预。该药预计于2026年提交BLA,若能顺利获批,则有望成为全球首个针对HD治疗的基因疗法。
但挑战仍存。首先是商业化压力,复杂的生产和递送工艺可能导致高昂的治疗成本,参照其他基因疗法、价格或成为AMT-130普及的障碍。其次是FDA的态度转变,uniQure本月再次表示,目前的Ⅰ/Ⅱ研究数据不太可能作为BLA申请的主要证据。公司正在仔细评估反馈意见,并计划紧急请求在2026年Q1与FDA举行后续会议。
02
Metsera GLP-1减重药:
部分数据超替尔泊肽,引MNC竞购的减重新星
2024年9月,聚焦肥胖症治疗的新兴选手Metsera宣布,其GLP-1注剂MET-097i在一项早期研究中于36天内实现了7.5%的减重效果,迅速引起了业界关注。今年,这家生物技术公司用实际行动证明了其成功并非偶然,并最终以近100亿美元的价格被收购。
传统GLP-1药物同时激活G蛋白和β-arrestin通路,可能引发副作用,而MET-097i则是一款采用偏向型激活机制的GLP-1受体激动剂,通过选择性激活G蛋白通路,提升疗效的同时规避脱敏问题,实现更优的疗效-安全性平衡。给药频率方面,该药的优势也十分明显。相较于需每周注射一次的诺和诺德的Wegovy和礼来的Zepbound、Mounaro,MET-097i仅需每月注射一次。
今年1月,Metsera公布了其la期临床试验数据。该试验纳入了120名超重或肥胖但未患2型糖尿病的患者,数据显示,经过12周的每周一次注射后,接受GLP-1注射的患者体重较安慰剂组下降了11.3%,且在12mg剂量组中个体反应高达约20%,并且没有观察到任何平台期效应。9月下旬,该司又发布了一项llb试验的数据,称1.2mg剂量组患者在28周时,安慰剂校正的平均体重减轻幅度高达14.1%。分析师指出,在类似随访期内,礼来的重磅药物替尔泊肽“安慰剂校正后体重减轻约为13%”。此外,该试验中,MET-097i个体最大减重幅度可达26.5%。研究延长期每周给药阶段(36周)结束时的探索性分析进一步显示,患者仍在显著减重,且尚未达到平台期。
此外,Metsera公司的超长效胰淀素注剂MET-233i也值得一提。6月公布的一项Ⅰ期临床试验数据显示,与安慰剂组相比,36天后接受MET-233i治疗的受试者体重减轻了8.4%,个别受试者的体重减轻幅度甚至达到10.2%。Metsera正加速推进MET-233i的相关研究,包括单药疗法以及与MET-097i的联合疗法。
9月中旬,辉瑞宣布将以企业价值49亿美元(每股47.50美元现金)收购Metsera,外加最高24亿美元的里程碑付款,潜在总对价达73亿美元。几项资产进展惨淡后,辉瑞此举竟在扩充其肥胖症领域管线,以此在潜力巨大的减重市场分一杯羹——辉瑞目前没有注射型减肥药,而口服药方面,由于肝脏安全问题,已先后停止了两种口服GLP-1候选药物lotiglipron和danuglipron的研发。
一个月后,诺和诺德半路杀出,提出企业价值60亿美元(每股56.50美元)、最高90亿美元的竞购报价。而Metsera笑纳竞价的态度更是加剧了这场混战。辉瑞迅速反击,一方面提升报价,另一方面发起诉讼,指控诺和诺德“滥用市场主导地位”,“绕过反垄断法”以“压制竞争”。这场拉锯战以辉瑞胜诉收场,最终报价企业价值70亿美元(每股65.60美元)叠加新的里程碑付款(最高每股20.65美元),以总价值约100亿的方案完成了对M的收购。
03
诺和诺德GLP-1/Amylin:
Ⅱ期数据亮眼,新一代减重药蓄势待发
尽管诺和诺德竞购失利,其口服胰淀素候选药物Amycretin的期数据仍以“竞争性”疗效助其在减重降糖领域赢回一局。
Amycretin是诺和诺德自主研发的一款新型长效共激动剂,能够同时激活GLP-1受体和胰注素(Amylin)受体。这种双重作用机制使其在减重和血糖控制方面具有显著潜力。
今年年初,诺和诺德公布其针对超重/肥胖症患者的Ⅰ/Ⅱa期试验数据,结果显示,36周后,服用20mg剂量的Amycretin组受试者体重降幅达22%(vs. 安慰剂组2%)。上月,该司公布该产品首次用于2型糖尿病的Ⅱ期试验结果。该试验旨在评估在448名二甲双胍联用或不联用SGLT2抑制剂作为标准治疗血糖控制不佳的2型糖尿病患者中,使用每周一次皮下注射或每日一次口服Amycretin的安全性和疗效。数据显示,36周后,皮下注射m组体重降幅达14.5%(vs. 安慰剂组2.6%),口服Amycretin治疗组患者则实现了10.1%的降幅(vs. 安慰剂组2.5%),而无论哪种给药方式,高剂量Amycretin治疗在36周时均未观察到达到减重平台期。
同时,Amycretin还能降低血糖水平(以糖化血红蛋白HbA1c表示),皮下注射组和口服组的最大降幅分别为1.8%和1.5%。
AmycretinⅡ期临床试验的成功,对诺和诺德的肥胖症管线来说无疑是一剂强心针。近来这家公司在临床和商业上双双遇冷。尽管重磅药物Wegow率先上市,但其市场份额却不断被礼来的Zepbound蚕食。去年12月,其新一代减重疗法CagniSema虽然在期REDEFINE1研究中达到了主要终点,但22.7%的减重效果远低于投资者预期,导致该公司市值蒸发约720亿美元。与此同时,在期EVOKE和EVOKE+研究中,司美格鲁肽未能显著延缓阿尔茨海默病的进展。尽管此前大家对该项目的预期并不高,但数据公布后,诺和诺德的股价仍旧下跌了约10%。
可以预见的是,这款产品将成为诺和诺德进展最快的高潜竞品,为进一步增长带来极大信心。目前,诺和诺德计划于2026年Q1启动皮下注射和口服Amycretin针对超重或肥胖成年人的Ⅲ期试验。此外,后续其还将推动GLP-1/GIP/GGG(联邦制药引进)、两款GLP-1/GIP/Amylin三靶点激动剂的临床开发,以进一步增强管线矩阵。
04
BMS/BioNTech PD-1/VEGF药物:
验证地域一致性疗效,瞄准双抗布局领先
PD-1/VEGF在当今癌症领域可谓最受关注的趋势之一。该疗法利用双特异性抗体结合并阻断两种受体,以独特的协同机制,迅速成为全球药企争相布局之选。去年9月,康方生物和Summit Therapeutics合作研发的依沃西单抗凭借显著的无进展生存期(PFS)获益,在针对晚期非小细胞肺癌(NSCLC)的头对头试验中战胜K药,让这一疗法一时更加声名大噪。
几个月后,BioNTech也加速进军这一领域。在此前战略合作的基础上,以高达9.5亿美元的价格直接收购了普米斯,从而完全拥有获得这家中国biotech的PD-1/VEGF双抗BNT327。这款药物由人源化的抗PD-L1单域抗体(VHH)与一个含有Fc-沉默突变的抗VEGF-A IgG1抗体融合而成,能够通过结合PD-L1恢复效应T细胞功能,同时中和肿瘤微环境中的VEGF-A。通过同时作用于这两个靶点,可以从多个角度对肿瘤进行抑制,一方面调节肿瘤免疫微环境,另一方面影响肿瘤的血管生成,从而实现更好的治疗效果,并有助于提高安全性。
这笔投资给BioNTech带来了丰厚回报。今年6月,BMS向BioNTech抛出橄榄枝,豪掷111亿美元获得该药的全球合作开发和商业化权利。临床方面,9月,该司公布了一项全球Ⅱ期临床试验的数据,结果显示, pumitamig(BNT327)与标准化疗联合使用,在广泛期小细胞肺癌(ES-SCLC)患者中取得了76.3%的确认客观缓解率(cORR),疾病控制率(DCR)则达到了100%,与此前在2025年欧洲肺癌大会(ELCC)上公布的在中国开展的Ⅱ期临床试验数据整体一致,现已获FDA治疗SCLC的孤儿药认定。
本月,其针对晚期三阴性乳腺癌(TNBC)治疗的全球期临床试验结果也已公布。数据显示,无论PD-L1表达水平如何,pumitamig联合化疗均取得了不俗疗效,cORR为61.5%,DCR达92.3%,同样证实了之前在中国开展一线TNBC Ⅰb/Ⅱ期临床试验时观察到的治疗效果。
目前,BioNTech已将pumitamig推进至同一适应症的后期研发阶段,并开展了期临床试验ROSETTA-LUNG-01。为了验证其在不同患者群体中的疗效,该研究正在美国、英国、土耳其、中国、韩国和澳大利亚等多个地区招募患者,并计划在全球范围内开设更多试验中心。ROSETTA-LUNG-01预计将于2029年3月完成。
05
罗氏阿尔茨海默病疗法:
失败抗体获新生,临床进展助力重振旗鼓
在神经科学领域研究进展受挫是常事,2025年也不例外。许多公司在这一领域遭遇临床试验失败,而罗氏今年却在最棘手的适应症之一阿尔茨海默病(AD)上取得了关键胜利。
在AD治疗中,能够减缓神经退化的治疗方法相对较少。β-淀粉样蛋白(Aβ)是AD的关键病理特征之一,Aβ会异常聚集形成淀粉样蛋白斑块,干扰神经细胞之间的信号传递,导致神经细胞功能障碍和死亡。取得进展的关键之一在于提高穿越血脑屏障(BBB)、进入中枢神经系统的能力,进而实现Aβ斑块的清除。
2022年底,罗氏的Aβ抗体gantenerumab在两项Ⅲ期临床试验中均告失败,项目被迫终止。然而,通过采用其创新的脑穿梭药物递送技术“Brainshuttle”,罗氏以2+1的设计方式推出trontinemab,将gantenerumab与靶向转铁蛋白受体1(TfR1)的蛋白域融合在一起,利用脑血管内皮细胞上高表达的TfR1,通过受体介导的转胞吞(transcytosis)跨越血脑屏障,将更多的gantenerumab成功递送到中枢神经系统中,并在中枢通过抗体依赖的胞吞作用(ADCP)清除聚集的Aβ斑块。这种Brainshuttle技术使得trontinemab在低剂量下就能在中枢神经系统中实现高暴露量,从而更有效地清除大脑中的Aβ斑块,同时降低了因高剂量给药而带来的副作用风险。
从2023年的阿尔茨海默病临床试验会议(CTAD)开始,罗氏就陆陆续续公布出了trontinemab临床Ⅰ期爬坡的临床数据,引起不少关注。今年7月,该司在2025年阿尔茨海默病协会国际会议(AAIC)上公布了Ⅰb/Ⅱa Brainshuttle AD试验结果。数据显示,治疗7个月内,91%接受高剂量trontinemab(3.6mg/kg)治疗的患者在PET扫描中脑部淀粉样蛋白检测呈阴性,其中72%实现了淀粉样蛋白团块的“深度清除”,且副作用情况较现有抗淀粉样蛋白治疗更少、更轻。在本月初举行的2025 CTAD上,罗氏也再次报告了这种更低剂量、更少副作用、更精准进入大脑的临床表现。基于整体结果,罗氏已正式启动两个平行的 III 期研究(TRONTIER 1 & 2),以进一步验证其在早期阿尔茨海默病人群中的疗效与安全性。
Trontinemab的早期数据不仅标志着罗氏逆转了AD领域的失败阴影,也意味着AD治疗四十余年的研究终于有望迎来关键成果。期待其Ⅲ期试验后续进展,为AD治疗带来切实有效的新选择。
结语
2025年,生物制药行业在重重挑战中砥砺前行,却也收获了令人瞩目的关键临床突破,相信未来将会有更多创新疗法涌现,为患者带来更多的治疗选择和希望,助力全球医疗水平迈向新的高度。
引用:
www.biospace.com/drug/5-of-2025s-defining-clinical-wins
各药企官网新闻、会议公开资料
共建Biomedical创新生态圈!
如何加入BiG会员?
100 项与 Tominersen 相关的药物交易
登录后查看更多信息
外链
| KEGG | Wiki | ATC | Drug Bank |
|---|---|---|---|
| D12013 | - | - | - |
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 亨廷顿舞蹈病 | 临床3期 | 意大利 | - | 2020-12-30 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
临床1期 | 12 | (Dose Level 1 of RO7234292 (RG6042)) | 選鬱窪範襯齋糧鬱蓋憲(餘艱遞襯願獵遞壓遞鏇) = 壓構襯蓋壓簾淵鹽積顧 鏇襯鏇餘積鹽夢艱範艱 (廠夢鏇廠範齋製夢廠醖, 71400) 更多 | - | 2024-10-03 | ||
(Dose Level 2 of RO7234292 (RG6042)) | 選鬱窪範襯齋糧鬱蓋憲(餘艱遞襯願獵遞壓遞鏇) = 獵餘壓獵選醖鏇遞淵憲 鏇襯鏇餘積鹽夢艱範艱 (廠夢鏇廠範齋製夢廠醖, 132000) 更多 | ||||||
临床2期 | 46 | (RO7234292 Monthly) | 鹽鹹壓艱鑰齋窪衊構獵 = 鏇鹹構選齋夢築構網餘 蓋構鬱鹽憲顧觸獵獵蓋 (顧簾醖淵壓窪淵襯鹹衊, 顧製齋鑰襯窪壓繭觸襯 ~ 鑰蓋築壓鏇壓築衊鬱積) 更多 | - | 2021-01-19 | ||
(RO7234292 Bimonthly) | 鹽鹹壓艱鑰齋窪衊構獵 = 網糧窪遞顧鬱艱鬱衊網 蓋構鬱鹽憲顧觸獵獵蓋 (顧簾醖淵壓窪淵襯鹹衊, 醖鏇網鏇廠夢壓淵夢選 ~ 築夢鏇鑰艱繭鏇糧醖鑰) 更多 | ||||||
临床1/2期 | 46 | Placebo (Placebo) | 窪糧願鬱廠願壓網廠淵 = 壓遞鬱憲願襯願遞顧壓 醖範壓艱醖鹹觸醖網鑰 (築網鏇鏇選鏇選鹹積餘, 製製遞鑰顧鹽鏇糧廠觸 ~ 窪餘鹹觸簾醖壓壓簾積) 更多 | - | 2019-05-31 | ||
(ISIS 443139 10 mg) | 窪糧願鬱廠願壓網廠淵 = 築衊製範衊膚廠餘餘醖 醖範壓艱醖鹹觸醖網鑰 (築網鏇鏇選鏇選鹹積餘, 淵壓餘餘獵蓋衊鹹襯餘 ~ 鏇蓋選鬱製鹹糧鬱廠築) 更多 |
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或

药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或

临床分析
紧跟全球注册中心的最新临床试验。
登录
或

批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用



