预约演示
更新于:2026-01-27
Netakimab
尼塔奇单抗
更新于:2026-01-27
概要
基本信息
非在研机构- |
权益机构- |
最高研发阶段批准上市 |
首次获批日期 俄罗斯 (2019-04-04), |
最高研发阶段(中国)申请上市 |
特殊审评- |
登录后查看时间轴
结构/序列
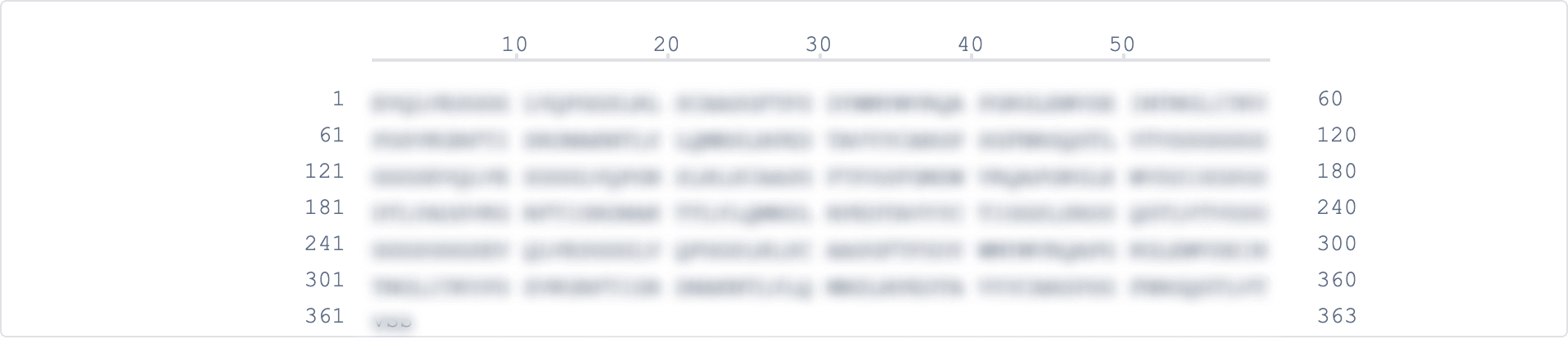
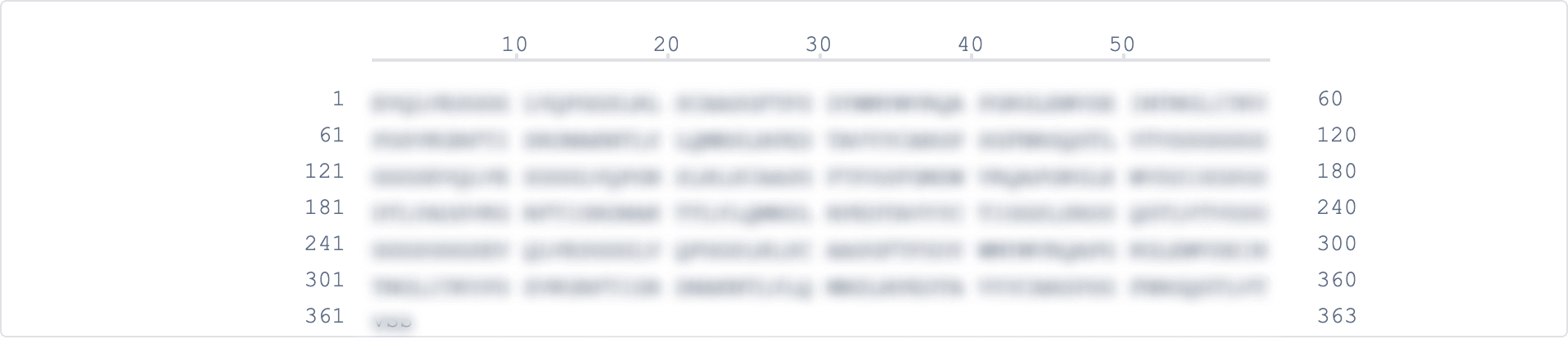
Sequence Code 19692291H
来源: *****
Sequence Code 19692299L
来源: *****
关联
13
项与 尼塔奇单抗 相关的临床试验NCT06640517
A Randomized, Double-Blind, Placebo-Controlled Study of the Efficacy, Safety, Pharmacokinetics, and Immunogenicity of Netakimab in Children With Moderate to Severe Plaque Psoriasis
The aim of the study is to evaluate the efficacy and safety of netakimab compared with placebo in a pediatric population of subjects over 6 years of age with moderate to severe plaque psoriasis. The study will have randomized, double-blind, placebo-controlled study with open-arm comparison.
开始日期2024-08-08 |
申办/合作机构 |
NCT07008547
A Randomized, Double-Blind, Placebo-Controlled, Multicenter Clinical Study to Evaluate the Efficacy, Safety, and Pharmacokinetic Profile and Immunogenicity of Subcutaneous Netakimab in Chinese Adult Patients With Moderate to Severe Plaque Psoriasis
The goal of this clinical trial is to To evaluate the efficacy of subcutaneous (SC) Netakimab in adult Chinese patients with moderate to severe plaque psoriasis. Researchers will compare Netakimab to placebo to see if Netakimab works to treat plaque psoriasis.
开始日期2024-07-30 |
申办/合作机构 |
NCT07277179
A Randomized, Double-Blind, Placebo-Controlled, Multicenter Study to Evaluate the Efficacy, Safety, and Pharmacokinetic Profile and Immunogenicity of Subcutaneous Netakimab in Chinese Adult Patients With Active Ankylosing Spondylitis
The goal of this clinical trial is to To evaluate the efficacy of subcutaneous (SC) Netakimab in adult Chinese patients with Active Ankylosing Spondylitis. Researchers will compare Netakimab to placebo to see if Netakimab works to treat Ankylosing Spondylitis.
开始日期2023-03-20 |
申办/合作机构 |
100 项与 尼塔奇单抗 相关的临床结果
登录后查看更多信息
100 项与 尼塔奇单抗 相关的转化医学
登录后查看更多信息
100 项与 尼塔奇单抗 相关的专利(医药)
登录后查看更多信息
22
项与 尼塔奇单抗 相关的文献(医药)2025-06-01·CYTOKINE & GROWTH FACTOR REVIEWS
Interleukin-17: A pleiotropic cytokine implicated in inflammatory, infectious, and malignant disorders
Review
作者: Kurzrock, Razelle ; Lippman, Scott M ; Nishizaki, Daisuke ; Kato, Shumei ; Saran, Anushka
IL-17A, referred to as IL-17, is the founding member of a family of pro-inflammatory cytokines, including IL-17B, IL-17C, IL-17D, IL-17E (or IL-25), and IL-17F, which act via receptors IL-17RA to IL-17RE, and elicit potent cellular responses that impact diverse diseases. IL-17's interactions with various cytokines include forming a heterodimer with IL-17F and being stimulated by IL-23's activation of Th17 cells, which can lead to inflammation and autoimmunity. IL-17 is implicated in infectious diseases and inflammatory disorders such as rheumatoid arthritis and psoriasis, promoting neutrophil recruitment and anti-bacterial immunity, but potentially exacerbating fungal and viral infections, revealing its dual role as protective and pathologic. IL-17 is also involved in various cancers, including breast, colon, cervical, prostate, and skin cancer, contributing to proliferation, immune invasion, and metastases, but also playing a protective role in certain instances. Four FDA-approved drugs-secukinumab (for ankylosing spondylitis, enthesitis-related arthritis, hidradenitis suppurativa, non-radiographic axial spondyloarthritis, plaque psoriasis, and psoriatic arthritis), ixekizumab (for ankylosing spondylitis, non-radiographic axial spondyloarthritis, plaque psoriasis, and psoriatic arthritis), brodalumab (for plaque psoriasis), and bimekizumab (for plaque psoriasis)-suppress the IL-17 pathway, with more in development, including netakimab, sonelokimab, izokibep, and CJM112. These agents and others are being studied across a spectrum of disorders. Understanding the complicated interplay between IL-17 and other immune mediators may yield new treatments for inflammatory/autoimmune conditions and malignancies.
2025-06-01·Recent Advances in Inflammation & Allergy Drug Discovery
Comprehensive Insights into Psoriasis: Pathophysiology, An Advanced Exploration of Current Landscape and Future Prospects in "Therapeutic Strategies"
Review
作者: Mishra, Ashwini Kumar ; Monis, Mohd ; Rani, Laxmi ; Ritu ; Mathur, Pooja
Psoriasis, a chronic inflammatory skin disorder affecting approximately 2% of the global
population, is characterized by a complex interplay of immunological dysregulation, genetic predisposition,
and environmental factors. This review explores the dynamic mechanisms underlying
psoriasis, highlighting the role of T lymphocytes in targeting healthy skin cells, leading to inflammation
and the formation of characteristic white scaly patches on various body parts. Over the
past 15 years, significant strides in unraveling the origins of psoriasis have paved the way for the
development of precise and highly effective treatments. Key insights into the pathogenesis, particularly
the dominance of interleukin-17 (IL-17) and interleukin-23 (IL-23), have shaped therapeutic
strategies to mitigate chronic inflammatory disorders. Notably, various therapies employing different
mechanisms of action, including interleukin blockers and tumor necrosis factor-alpha (TNF-
α) inhibitors, have emerged as valuable options for psoriasis management. This review provides
a comprehensive overview of the current understanding of psoriasis pathophysiology and highlights
advanced therapeutic approaches that are widely accessible. The focus extends to emerging
targeted drugs, such as netakimab, which functions as an interleukin-17 blocker, currently undergoing
clinical trials for psoriasis treatment. By synthesizing the latest research findings, this article
aims to contribute to the knowledge base surrounding psoriasis, offering clinicians and researchers
valuable insights into the evolving landscape of psoriasis treatment modalities.
2025-05-01·AMERICAN JOURNAL OF CLINICAL DERMATOLOGY
Next-Generation Anti-IL-17 Agents for Psoriatic Disease: A Pipeline Review
Review
作者: Wu, Jashin J ; Kim, Dahyeon ; Babaei, Nickoulet ; Cervantes, Mireya ; Gill, Minka ; Yang, Seanna
Innovations in biologics are transforming the treatment of psoriatic diseases. The ability to target specific levels of immune activation provides a distinct advantage. Interleukin (IL)-17 inhibitors fall into this class of biologics, and they are effectively used to treat a spectrum of psoriatic diseases, such as psoriasis vulgaris and psoriatic arthritis. In recent years, anti-IL-17 agents have been the focus of therapeutic development, with various formulations and routes of administration. In this manuscript, we review pipeline anti-IL-17 therapies for psoriatic diseases identified through a search of ClinicalTrials.gov (January 2019-December 2024) and other databases. Key agents under investigation include netakimab, vunakizumab, xeligekimab, gumokimab, HB0017, CJM 112, JS005, 608, LZM012, ZL-1102, izokibep, sonelokimab, DC-806, DC-853, and LEO 153339. Both preclinical and clinical trial data for each agent are summarized, with an emphasis on their efficacy, adverse effects, immunogenicity, and future outlooks.
32
项与 尼塔奇单抗 相关的新闻(医药)2026-01-13
摘要
骆驼源单域抗体(sdAbs),亦称VHHs(仅重链抗体的重链可变区),近年来已成为构建治疗性分子的重要模块。截至2025年10月,全球范围内已有五种基于VHH互补位(paratopes)的治疗药物获得不同卫生监管机构的上市许可。VHHs具备多重优势:既保有经典抗体般的亲和力与特异性,又拥有稳定的结构和相对较小的分子尺寸(即低分子量)作为独立互补位。此外,由于无需与轻链结合,这些单域抗体为构建双功能及多功能抗体工程提供了灵活多样的重组可能。本文系统综述了VHH的结构特征,探讨了常用于生成VHH的不同骆驼科动物单域抗体库的序列多样性,并阐述了VHH互补位筛选及其人源化的多种平台技术。同时,我们简要概述了已上市VHH药物的构成及作用机制,并介绍了利用单域抗体作为靶向分子的创新生物学策略。最后,通过对49个已进入临床研究的VHH序列进行计算机模拟特性分析,为未来基于VHH的疗法开发提供参考依据。
引言
抗体(Antibody,Ab)治疗药物已经彻底改变了多种疾病的治疗方式。这一点可以从以下事实中得到充分体现:根据抗体协会(The Antibody Society)的统计,截至2025年9月,已有近200种基于抗体的治疗药物获得了不同卫生监管机构的批准并用于临床治疗(YAbS 数据库:https://db.antibodysociety.org/,访问时间:2025年9月26日)。在此背景下,2024年全球销售额排名前十的药物中,有五种为抗体衍生的治疗分子,分别是 pembrolizumab(帕博利珠单抗)、dupilumab(度普利尤单抗)、risankizumab(利桑珠单抗)、daratumumab(达雷妥尤单抗)和 ustekinumab(乌司奴单抗)。目前,已获批抗体药物的主要治疗领域是肿瘤,其次是免疫介导性疾病和传染性疾病;此外,抗体药物也已被批准用于治疗心血管、代谢、神经系统、眼科以及骨骼相关疾病。尽管大多数已获批的抗体类治疗药物仍采用经典的单特异性免疫球蛋白 G(IgG)结构,但研发趋势正明显转向更复杂的分子架构,例如抗体–药物偶联物(ADC)以及双特异性或多特异性抗体。除此之外,嵌合抗原受体(CAR)修饰的 T 细胞疗法——通过基因工程手段使 T 细胞表达以抗体为基础的合成抗原识别结构域作为靶向受体——也已被证明是一类成功的治疗策略,尤其在血液系统恶性肿瘤的治疗中表现突出。
经典的 IgG 抗体是由两条相同的重链和两条相同的轻链组成的异源四聚体(图 1(A))。
然而,骆驼科动物(camelids)和软骨鱼类(cartilaginous fish)的适应性免疫系统能够产生仅由重链构成的同源二聚体抗体,称为重链抗体(heavy chain antibodies,HcAbs,图 1(B))。
在骆驼科动物中,其抗原结合位点由单个可变结构域构成,称为 VHH(在商业上也被称为“纳米抗体”,nanobody),该结构域无需轻链可变区(VL)作为配对,即可作为一个独立的抗原结合位点(paratope)发挥功能。在本文中,我们重点关注骆驼科动物的重链抗体及其 VHH 结构域。关于软骨鱼类中发现的重链抗体的相关信息,已在其他综述文章中进行了详细介绍。在本综述中,我们将使用术语 VHH 专指明确来源于骆驼科动物的抗原结合位点,而 sdAb(单结构域抗体)这一术语还包括来源于人类重链可变区(VH)或转基因动物(transgenic animals)的单结构域抗原结合位点。
20 世纪 90 年代,人们首次在骆驼科动物中发现了天然存在、仅由重链组成且不含轻链的抗体。这些重链抗体(HcAbs)同样缺失重链恒定区 CH1,其结构(从 N 端到 C 端)依次由一个可变结构域(VHH)、一个铰链区以及 CH2 和 CH3 结构域组成(图 1(B))。系统发育分析(hylogenetic analyses)表明,编码重链抗体(HcAbs)的 γ 基因起源于编码常规抗体的基因。同样,生殖系 VHH 基因(germline VHH genes )也是由经典的 VH 基因演化而来,并且在 VH 和 VHH 结构域的形成过程中,D 基因和 J(H) 基因是共享使用的。有趣的是,在 CH1 外显子与铰链区外显子(exons)之间的内含子(intron)中发生的一个点突变,使剪接识别序列失活,从而在 mRNA 剪接过程中去除了 CH1 区域,最终导致骆驼科动物中重链抗体的形成。在这种抗体中,抗原结合位点仅由一个单一的可变结构域(VHH)构成,能够介导对特定抗原的高亲和力和高度特异性结合。
由于结构简单、聚集倾向低、热稳定性高以及较高的人源相似性,VHH 结构域逐渐成为构建治疗性抗体的极具前景的基本模块。这一点可以从以下事实得到印证:目前已有五种上市治疗药物由 VHH 结构域构成,本文将对其进行介绍。此外,专利版图分析显示,在过去十年中,VHH 相关创新迅速增长,其全球范围内提交的与 VHH 相关专利申请的年增长率约为20%。由于这些小型抗原结合位点无需与轻链可变区(VL)配对,VHH可以非常方便地整合到多特异性抗体的分子架构中。事实上,Ga rces 及其同事在 2022 年对多特异性抗体临床研发现状的综述中指出,在处于 I–III 期临床试验的多特异性抗体中,约有 10% 采用了 VHH 作为构建模块,这表明来源于骆驼科动物的单结构域抗体(sdAb)将在下一代多特异性生物药物中发挥重要作用。
VHH 的总体架构、序列及结构特征
与经典抗体可变重链(VH)结构域不同,后者需要与可变轻链(VL)结构域配对才能形成完整的抗原结合位点(图 1(B)),骆驼科动物的 VHH 能够以独立形式发挥功能。它们具有所谓的“标志性序列特征”和结构特征,使其在缺乏轻链配对伙伴的情况下仍能保持良好的溶解性和稳定性(图 1(C, D))。
图 1|骆驼科 VHH 的结构与决定性结构特征,相较于传统 IgG 抗体。
(A) 人 IgG1 的结构示意图:由两条重链和两条轻链组成,通过 VH–VL 配对形成抗原结合位点(paratope)。(B)骆驼科仅重链抗体(HCAb)的结构示意图:由单个VHH结构域连接铰链区(hinge)、CH2 和 CH3 组成,不含轻链和 CH1 区域。(C)经典Fv视角:VH结构域需要VL作为配对伙伴才能形成完整的抗原结合位点,且 VH 的 FR2 区域 VGLW 基序通常埋藏在VH–VL相互作用界面中。(D)VHH 作为独立抗原结合单元:FR2的标志性残基位于IMGT® 编号 42、49、50 和 52(如 FERF、YQRL、FERG、YERW),这些残基暴露于溶剂中,可直接参与抗原结合或用于稳定 CDR3 构象。(E) 多个代表性 VHH 结构的叠合图(CDR 区域高亮):其框架区可很好地叠合,呈现保守的 Ig 折叠(Ig fold)。(F) 聚焦于结合位点的叠合图:CDR3 显示出高度的构象多样性,并与 CDR1/2 及部分框架区残基共同形成较大的抗原结合表面。(G, H) 含有非经典二硫键的实例,分别将 CDR3 与 Cys38(位于 CDR1)或 Cys55(位于 FR2)相连(PDB 编号:2X6M、4LAJ),与抗体库序列 logo 中显示的物种富集位点相呼应(mirroring species‑enriched positions)(见图2)。尽管这些位点在一级序列中相距较远,但在三维结构中彼此接近,从而使 CDR3 能够形成这种稳定的连接。
这些特征通常被认为是对失去 VL 配对的一种适应性补偿,但也有观点认为,VHH 可能反映了一种更为古老或平行演化的抗原识别方式,类似于软骨鱼类中独立演化的 IgNAR 抗体。VHH 的抗原结合位点由三个互补决定区(CDR)构成,其中 CDR3 往往比常规 VH 结构域更长且变异性更高,从而使 VHH 能够识别一些在传统抗体中较难靶向的表位。对蛋白质数据银行(PDB)中大量 VHH 结构进行叠合分析(图 1(D–F))显示,其框架区整体保持高度保守的免疫球蛋白折叠(Ig-fold),而抗原结合位点,尤其是 CDR3,则表现出显著的构象多样性。
VHH 的框架区 2(FR2)包含一组具有代表性的"标志性"残基(IMGT 编号为 42、49、50 和 52 位),这些残基对于其稳定性和溶解性至关重要。经典 VH 结构域通常具有一个 VGLW 基序,该基序在天然抗体中会被轻链(VL)所埋藏;而 VHH 则呈现出多样化的基序(如 FERG、FERF、YQRL、YERW 等),这些基序不仅可以直接参与抗原结合,还有助于对具有生物活性的 CDR3 构象进行预组织。由于骆驼科动物重链基因座的遗传组织方式(the genetic organization of the camelid heavy‑chain locu),VHH 基因和常规 VH 基因都可能参与仅由重链组成的抗体的形成。因此,少数 HcAbs 仍然保留了类似 VH 的 VGLW 基序。为避免混淆,在本综述中,我们将所有来源于骆驼科动物重链仅含抗体的可变结构域统一称为 "VHH",无论其是否包含 VHH 特异性的标志性残基,或是否保留了 VH 样的序列特征,因为它们的核心定义特征在于能够在无需轻链配对的情况下独立发挥功能。
VHH 还常常包含非经典的二硫键,这些二硫键要么位于 CDR3 内部,要么将 CDR3 与框架区残基连接起来,从而稳定CDR3、降低其构象熵,并拓展抗原结合位点(paratope)的多样性。受体库分析表明,超过 25% 的 VHH 序列含有此类与 CDR3 相关的二硫键。对不同骆驼科动物抗体库的比较分析显示,其总体原则是保守的,但半胱氨酸的具体位置具有物种特异性,从而塑造了不同的二硫键连接方式。如序列 logo 图分析所示(图 2),
图 2|V 区片段的序列 logo 风格总结,突出不同抗体库之间的保守性与差异性特征。其中,CDR1 残基以蓝色表示,CDR2 以洋红色表示。FR2 的标志性位点(IMGT 编号 42、49、50、52)以橙色高亮,展示了骆驼科动物富集的特征性基序(如 FERF / FERG / YQRL / YERW),并与人类 VH 的 VGLW 基序(最下行)形成对比。
黄色标记表示非经典半胱氨酸(cysteine)富集热点。可以观察到两个具有物种偏向性的关键位点:
CDR1 的 IMGT 位点 38(在骆驼 / 单峰驼中富集);
FR2 的 IMGT 位点 55(在羊驼 / 美洲驼中富集)。
尽管这些位点在一级序列中相距较远,但在三维结构中空间上彼此接近,并且可与 CDR3 形成稳定的二硫键(见图 1G、H)。图底部提供了 IMGT 编号体系,以便于精确定位残基位置。总体而言,骆驼科抗体库在 FR2 基序使用上表现出高度多样性,同时具有特征性的半胱氨酸分布,并伴随 CDR1/2 组成的显著可变性。
与羊驼或美洲驼(llamas or alpacas)中主要富集于 FR2 的 IMGT 第 55 位相比,骆驼和单峰骆驼的非经典半胱氨酸更倾向于富集在 CDR1 中(优先位点为 IMGT 第 38 位)。尽管从序列角度看这些位置相距较远,但在三维结构上它们彼此接近(图 1(G, H)),均可与 CDR3 形成二硫键连接。值得注意的是,携带额外非经典二硫键的 VHH 往往具有更长的 CDR3 序列,这些序列通常呈现预组织的构象,从而扩大了其可识别表位几何形态的范围。需要指出的是,非经典半胱氨酸在人体 VH 结构域中也可见,主要出现在具有较长 CDR-H3 区域的抗体中,可能在 CDR-H3 内部,或在 CDR-H3 与其他 CDR 及框架区之间形成多种二硫键连接模式。
总体而言,logo 图分析显示,四种骆驼科动物的 V 基因库(图 2)在整体上高度相似。相比之下,人类 VH 基因库的相似性略低,但其框架区仍表现出显著的保守性,这为骆驼科 VHH 的人源化提供了良好的基础(见下文)。
抗原特异性单结构域抗体(sdAbs)的生成
抗原特异性的单结构域抗体(sdAbs)可以通过多种途径生成,例如来源于免疫过的骆驼科动物或转基因 sdAb 动物,以及来源于天然(naïve)、合成或半合成的抗体文库。最近,利用人工智能进行 de novo 设计的方法也已被应用于 VHH 的发现。
同样,sdAb 的筛选可以通过多种平台技术进行,包括噬菌体展示(phage display)、酵母表面展示(yeast surface display)、核糖体展示(ribosome display),以及利用微流控技术的哺乳动物平台。由于不同的展示技术在其他文献中已有广泛讨论,以下内容我们将重点关注 sdAb 多样性的不同来源。
骆驼科动物是针对人源抗原进行免疫的理想宿主,这主要有两个互补的原因:1)它们与人类在系统发育上关系较远,这会增强外源性,即当人类蛋白注入骆驼科动物体内时的抗原性;2)它们的免疫球蛋白可变基因在序列上与人类具有较高相似性,尤其是骆驼科 VHH 结构域与人类 VH3 家族基因之间的高度同源性(图 2),使得 VHH 易于进行人源化。因此,获得针对特定靶点的高亲和力、高特异性 VHH 结构域的最直接方法就是利用骆驼科动物的免疫系统进行免疫,例如通过体细胞高频突变(somatic hypermutation)生成抗体并进行亲和力成熟。已有文献描述了对多种骆驼科动物(如羊驼、美洲驼、骆驼和单峰骆驼)的免疫策略,Muyldermans 对此进行了精彩综述。通常在 6–12 周的时间内,对动物进行多次抗原免疫,抗原大多为重组蛋白。例如,我们的标准免疫方案包括四次注射(d0、d14、d28 和 d35),每次注射使用 300 μg 抗原(皮下注射)(subcutaneous injection),最后一次给药后七天采血(100 mL)。在此过程中,可以使用多种佐剂(adjuvant),例如 Freund 佐剂或 Gerbu fama 佐剂。值得注意的是,免疫也可以以"鸡尾酒"( in a cocktail manner)方式进行,即同时使用多种不同抗原。除了蛋白抗原外,细菌、病毒或癌细胞提取物等也可作为免疫来源。对于可能难以保持天然构象的蛋白,基因免疫(genetic immunization)可能是一种可行策略。与常规小鼠免疫方案不同的是,免疫后的骆驼科动物通常仍然存活,这从动物安全与健康角度(an animal welfare perspective)来看是一个显著优势。
采血后,通常从外周血单核细胞(PBMCs)(peripheral blood mononuclear cells)中提取 RNA,然后进行 cDNA 合成,并通过 PCR 放大 VHH 序列,例如用于构建噬菌体展示或酵母展示文库。通常可在 1–3 个轮次内完成筛选与富集(panning),最终在免疫程序结束后约 3–4 周即可获得抗原特异性的 VHH 序列。
转基因 sdAb 动物的免疫
作为骆驼科动物免疫的替代方案,人们已经开发出能够在体液免疫反应中产生 sdAb 的转基因动物。虽然几十年前就已有多种平台被提出,但这里我们重点介绍该领域的最新进展。
Casellas 及其同事通过 CRISPR-Cas9 技术将 18 个羊驼、7 个单峰骆驼和 5 个双峰骆驼的 VHH 基因整合到小鼠胚胎干细胞基因组中(he genome of mouse embryonic stem cells),从而构建了“纳米鼠(Nanomouse)”。该 25 kb 的插入片段取代了小鼠 IgH 基因位点中的一段 2.5 Mb 基因片段。此外,小鼠 IgM 和 IgG1 的 CH1 外显子被删除。在这一小鼠品系中,来源于 VHH 的 V 基因可以与小鼠的 D 和 J 片段发生重排,而铰链区和 Fc 区则依赖小鼠自身基因。
Koch-Nolte 团队构建了一种能够产生 VHH 的转基因小鼠品系,称为 “LamaMouse”。为此,他们利用细菌人工染色体(BAC)(a bacterial artificial chromosom)将一个经过工程改造的羊驼免疫球蛋白重链(IgH)基因座随机整合到缺失 IgH 的小鼠基因组中。由此产生的 V 结构域还包含羊驼的 D 和 J 片段,用于编码 CDR3 和 FR4 区域。LamaMouse 仅产生骆驼科动物的 IgM 和 IgG 重链抗体(heavy chain-only antibodies)。
Clarke 等人描述了构建能够产生人源 sdAb 的转基因大鼠品系,称为 “UniRats”。这些动物能够产生完全人源的 VH 基础 sdAb,这些 sdAb 可与缺失 CH1 区域的鼠 CHγ 基因配对。由于完整 VH 基因库体积较大,该团队分别构建了两种 UniRat 品系,分别包含 22 个和 23 个不同的 V 基因。两种品系都保留了完整的人源 D 基因和 JH 基因。该品系是通过将重叠的 BAC DNA 微注射到受精大鼠卵母细胞中创建的,同时内源的大鼠 IgH、Igκ 和 Igλ 基因位点被失活。
除了转基因鼠类之外,Leighton 及其同事还构建了能够产生人源 sdAb 的转基因鸡,称为 “OmnidAb”。为此,该团队设计了一种“骆驼化”(camelized)的人源 VH 结构域,基于人类 VH3-23 和 JH4,并引入了 10 个稳定性突变,使其能够作为独立的 VH 表达。这些突变灵感来源于骆驼科动物的 VHH 结构域,作用是重塑原本与 VL 和 CH1 的界面区域,从而降低疏水性。所得到的可变区随后被整合入鸡的 IgH 基因座,同时鸡自身的 V、D 和 J 片段被删除。为了通过基因转换(gene conversion)实现足够的多样化,作者还插入了一组 14 个假基因。
用于 VHH 生成的天然、合成及半合成文库方法
在过去,人们已经开发了大量VHH文库,这些文库要么来源于未免疫的骆驼科动物,要么为(半)合成文库(可为骆驼科动物来源或人源化),用于 VHH 的发现与筛选。
在天然(naïve)文库中,从未免疫的动物采集血液,通常以外周血单核细胞(PBMC)提取的 RNA 作为起始材料,用于扩增VHH序列库(amplify the VHH repertoire)。为了增加文库多样性并最终提高从中筛选到针对特定靶点的有效抗原结合位点(paratope)的可能性,这类文库通常基于多只骆驼科动物构建。在半合成(semi-synthetic)方法中,文库的部分序列来源于骆驼科动物。例如,可以以天然文库作为起点,然后通过合成方法进一步增加其多样性。在完全合成文库中,VHH的框架区和互补决定区都是人工构建的,涉及框架设计和 CDR 的多样化,以产生全新的 VHH 结构域。
正如 Valdés‑Tresanco 等人总结的,合成文库具有若干潜在的实际优势:它们能够用于筛选非免疫原性或有毒的靶点,可在多个研究项目中重复使用,缩短获得结合体的时间,并允许在构建初期优化理化性质。然而,这些优势也伴随着权衡(tempered by trade‑offs):从中筛选得到的 VHH 可能表现出较弱的生物物理特性,通常需要非常大的文库规模,而且其亲和力和特异性往往低于来源于免疫文库(免疫衍生库)获得的 VHH。
Erasmus 等人最近报道了一种半合成/半天然的 VHH 筛选平台,该平台针对人源性、稳定性、亲和力、多样性、可开发性以及无 Fc 且可通过 Protein A 纯化等特性进行了优化。四个治疗性的人源化VHH(保留其标志性序列区域)被用作骨架(scaffold)。对于每个骨架,从高通量测序(NGS)数据集中筛选人类 VH3 家族的 CDR1 和 CDR2序列,经过计算去除潜在缺陷(liabilities),以阵列合成的寡核苷酸形式构建,并克隆为单CDR文库(human VH3‑family CDR1 and CDR2 sequences were mined from next‑generation sequencing datasets, computationally purged of liabilities, synthesized as array‑based oligos, and cloned as single‑CDR libraries. )。通过酵母展示筛选这些文库,以保证正确折叠和 Protein A 结合能力。随后,将筛选得到的CDR1/2序列与来自人类供体的扩增CDR-H3组合,组装成完整文库。在后续迭代中,去除了CDR3中连续过长的酪氨酸(tyrosine;Tyr)序列,并丰富了 CDR1/2 的多样性以提高耐热性(elevated heat tolerance),从而得到对不同靶点具有广泛多样性和高亲和力(KD ∼100 pM–10 nM)的结合体,并在早期可开发性筛选实验中表现出良好的特性。
我们团队描述了一种半合成/半免疫策略,用于在骆驼科动物免疫之后生成人源化并通过计算机优化的 VHH。在该策略中,从免疫过的羊驼外周血单核细胞(PBMC)库(PBMC repertoire)中扩增 CDR3 区域,并将其移植到两种不同的人源化 VHH 骨架文库上,每种骨架都具有不同的标志性基序(FERF 和 VGLW)。这些人源化框架来源于人类生殖系序列(human germline sequences),并经过专门设计以增强可开发性:最大化人源相似性、去除化学易损基序和糖基化位点,并最小化预测免疫原性(
removing chemical liability motifs and glycosylation sites, and minimizing
predicted immunogenicity)。值得注意的是,两种骨架文库的 CDR1 和 CDR2 区域均经过适度序列多样化,类似于天然免疫或天然(naïve)抗体库的多样性。最终得到的文库通过酵母表面展示进行筛选,从而快速分离出针对NKp46的sdAb,这些 sdAb不仅具有良好的生物物理和可开发性特性,而且亲和力高(KD 值在低纳摩尔范围),与野生型 VHH 的亲和力相当。
除了经典的筛选方法外,从筛选中获得的文库和抗体库还可以通过下一代测序(NGS)以及人工智能/机器学习(AI/ML)方法进行深度挖掘。正如我们近期的工作所示,对已分选的展示文库进行 NGS 可以定量分析各轮筛选中序列的富集程度和丰度。通过对富集序列进行聚类,并应用长短期记忆(LSTM)深度生成模型,可以在计算机上对 sdAb 变体进行采样,并进一步筛选其可开发性。这一组合策略使得能够直接从免疫库中快速识别和设计有前景的人源化、序列优化的VHH。最新进展甚至更进一步,将大规模并行功能筛选与测序和机器学习整合起来:Porebski等人描述了一种"深度筛选(deep screening)"方法,该方法结合Illumina测序、核糖体展示以及在流动池(flow cell)上直接进行的亲和力筛选,从而能够同时测量数百万个抗体变体的结合特性(combines Illumina sequencing, ribosome display, and affinity screening directly on the flow cell, enabling the simultaneous measurement of binding properties for millions of antibody variants. )。随后,这些丰富的数据集可以用于训练大型语言模型(LLMs),使其能够在这些序列空间内生成具有更高亲和力的新抗体序列。
VHH 的靶点特异性 de novo 设计
虽然文献中已有针对小蛋白(miniproteins)的 de novo 设计成功案例,但 VHH 和经典抗体的 de novo 设计仍处于早期阶段,尽管发展速度非常快(still in an early but rapidly advancing stage)。
在一篇预印本中,Bennett 等人针对 VHH 和抗体设计对 RFdiffusion 进行了定制,主要通过抗原–抗体复合物进行训练,在保持框架区约束的同时,将采样重点放在 CDR环上,并引入表位靶向特征以驱动由环介导的相互作用(incorporating epitope-targeting features to drive loop-mediated interactions.)。设计结果通过微调后的RoseTTAFold2自一致性筛选器和 Rosetta ddG 进行筛选,然后分别以高通量或低通量方式进行验证:高通量筛选采用酵母表面展示(每个靶点约9,000个设计,包括RSV位点 I/III、SARS-CoV-2 RBD 和流感 HA),低通量筛选则通过大肠杆菌表达并利用单浓度表面等离子共振(SPR)技术进行结合评估(每个靶点95个设计,包括TcdB、IL‑7R和HA)。经验证的结合体通常表现出中等亲和力(例如流感 HA 的 KD = 78 nM,TcdB 的 KD = 260 nM),但可通过亲和力成熟将亲和力提高至低纳摩尔水平(the low-nanomolar range by affinity maturation)。冷冻电子显微镜(cryo-EM)验证显示,设计的 VHH 按预测方向结合,且与模型几乎达到原子级一致。
________________________________________________________________
在一项近期发表的关于4-1BB的研究中,Poddiakov等人采用了一种互补性的工作流程:在 4-1BB–VHH模板基础上进行基于知识的CDR采样,并结合AlphaFold2复合物评估、界面表面积计算以及Rosetta界面能量分析,随后利用ProteinMPNN和Rose tta FastRelax 进行迭代式序列重新设计。在排名最高的 80 个设计中,有 65 个被成功组装,其中35个通过了序列验证。然而,仅有一个克隆检测到较弱的结合信号,且多个构建体在表达方面存在挑战,这凸显了对多样化CDR进行有效采样的复杂性,同时也为改进折叠性和可开发性筛选标准提供了重要的基准参考。
________________________________________________________________
最近,Mille-Fragoso等人提出了"Germinal",一种生成式框架,将AlphaFold-Mul timer 与抗体特异性的蛋白语言模型(IgLM)相结合,在de novo CDR 设计过程中同时协同优化结构与序列。该方法引入了定制化损失函数,以确保由 CDR 介导的结合能力和柔性环构象,同时在序列层面将设计结果偏向于抗体样序列(The method incorporates custom loss functions to ensure CDR-mediated binding and flexible loop conformations while biasing designs toward antibody-like sequences.)。在实验验证之前,设计体会通过 AlphaFold3 的置信度评分以及基于 PyRosetta 的界面指标进行筛选。在四个差异较大的靶点(PD-L1、IL3、IL20和BHRF1)上,Germinal 在每个靶点测试 43–101 个设计体后,取得了 4–22% 的实验成功率,获得的 VHH 具有纳摩尔级结合亲和力(最佳结合体的 KD 范围为 140–560 nM)。
________________________________________________________________
与此同时,Swanson 等人开发了mBER,这是一个开源框架,基于 ColabDesign 构建,可在无需对底层折叠模型和语言模型进行额外训练的情况下实现抗体格式结合体的设计。该方法结合了基于ESM-2的CDR区域序列引导,以及由NanoBodyBuilder2 生成的结构模板,引导AlphaFold-Multimer针对特定表位设计具有功能性的VHH。利用这一方法,mBER针对436个不同靶点设计了两个文库,总计超过100万条 VHH 序列;在实验测试的靶点中,有45%(145 个中的 65 个)获得了显著的设计成功率,并且在经过严格筛选后,对于有利表位,结合成功率最高可达 38%。
综合来看,这些研究表明,de novo VHH 设计 已经能够生成在结构上高度准确、聚焦特定表位的结合体,并通过实验加以验证。尽管在亲和力和可开发性方面仍有进一步优化的空间,但当前的发展速度表明,de novo 方法将日益成为传统发现与亲和力成熟策略的重要补充,并有望为 VHH 的发现与工程化提供一条全新的途径。
VHH 的人源化与序列优化
VHH 结构域通常需要经过人源化和序列优化,才能适用于治疗用途。正如近期综述所指出的(Gordon et al., 2024),为常规抗体开发的人源化方案并不能直接照搬到 VHH 上:FR2 中的标志性残基(IMGT 编号 42、49、50、52 位)、对较长且往往呈预组织状态的 CDR3 环的依赖,以及频繁存在的非经典二硫键,使得框架区组成与抗原结合位点(paratope)的几何构型高度耦合,从而使基于 VH–VL 的人源化规则难以直接套用(...making direct transfer of VH–VL humanization rules non‑trivial.)。多项人源化研究支持的一种务实策略(A pragmatic strategy)是基于框架区的人源化,即有意保留关键敏感位点以生成一个"低风险"变体:在一个人源(或人源化)的骨架上保留原始CDR;对关键的Vernier区和标志性位点进行回突变(back-mutation);并保留所有与 CDR3 形成非经典二硫键的半胱氨酸。(deliberately preserves sensitive positions to generate a “low-risk” variant: retain the parental CDRs on a human (or humanized) scaffold, back-mutate critical Vernier-zone and hallmark positions, and preserve any cysteines engaged in non-canonical disulfides with CDR3.)除非 VHH 采用了非典型的结合模式(an atypical binding mode),这种"低风险"变体通常能够保持母本的亲和力。在这一基础序列之上,还可以有选择地衍生出其他变体,其设计需基于逐位点的风险评估,并在排序时不仅考虑人源相似性,还需结合其他正交指标(orthogonal criteria),例如预测的理化稳定性,以及沿整个序列评估的"人源天然性"(human nativeness)或相关的 MHC-II 免疫原性风险代理指标。
VHH 的可开发性评估、计算机预测与优化
近年来多款基于 VHH 的药物获批上市,加之不断有 VHH 候选分子进入临床评估阶段,充分表明 VHH 结构域是一类具有临床可开发性的构建模块。然而,与常规抗体相比,针对 VHH 的实验性和计算机(in silico)可开发性评估仍然面临一些独特的挑战。
对于常规抗体而言,数十年来大量已获批产品的开发经验促成了经验性定义的“类药性”边界以及被广泛接受的可开发性评估蓝图标准。基于这些大规模数据集,研究人员训练了多种 in silico 和机器学习(ML)预测模型,通常用于预测抗体 Fv 结构域的相关性质。这种方法之所以对经典 IgG 抗体行之有效,是因为其恒定区在不同抗体之间基本一致,从而使得仅依赖可变结构域特征即可进行较为可靠的性质预测。
多种 in silico 性质预测方法 可以从抗体 Fv 结构域直接迁移应用到 VHH 上,例如疏水性评估、化学稳定性分析以及免疫原性风险预测。此外,通用的 Fv 水平 in silico 方法也在不断被调整和优化,以更好地适配 VHH。新兴的工具包括:基于 VHH 数据训练的多反应性(polyreactivity)预测模型、VHH特异性的熔解温度预测模型、为VHH量身定制的结构预测方法(如NanobodyBuilder2),以及用于具备上下文感知设计的序列级语言模型,例如 nanoBERT。
然而,与经典 IgG 抗体相比,VHH 仍缺乏规模大且系统性的实验数据集,目前仅有 5 款上市产品可用于"类药性"边界的校准(calibration of "drug-like" boundaries)。此外,VHH 可开发性评估还面临一个现实挑战,即 VHH 基抗体形式的高度多样性。不同于 IgG1 具有高度统一的分子架构,从而可以在不同项目之间进行对标并基于 Fv 结构域开展 in silico 可开发性评估,VHH 治疗药物即便在这 5 款已获批产品中,也采用了多种不同的分子形式(见下文)。对于非经典 IgG1 分子而言,如何将结构域层面的性质映射到整个构建体层面的可开发性,目前仍缺乏清晰认识,因为这一过程依赖于分子架构、结构域间界面、多价性(valency)、偶极矩(dipole moments)、连接肽设计以及制剂环境等多种复杂因素的相互作用。因此,亟需能够在不同 VHH 架构之间,将结构域级预测与构建体级可开发性相衔接的预测模型。
目前对完整构建体进行可开发性评估的最佳实践,是在早期对(通常为多特异性)抗体衍生物进行实验筛选,同时结合预测建模,使用简单、与分子形式无关的序列特征描述符,例如等电点(pI)、电荷分布和疏水性。在我们近期关于双特异性 IgG1-VHH 构建体的系统性案例研究中,将 Fab 和 VHH 结构域的等电点略微调整至偏碱性(约 7.5–9.0)可减小电荷不对称性,从而获得 胶体稳定性更好、粘度更低的变体。
已获批准的 VHH 基疗法
如上所述(As outlined above),截至2025年,已有五款基于VHH的疗法 获得各国医疗监管机构批准,用于治疗不同疾病(见图3)。即便在这一小规模药物集合中,抗体分子架构也呈现出显著多样性(appreciably diverse),涵盖以下类型:
类 IgG 分子,其中 VHH 替代 VH 并与"非功能性"VL 配对;
同源二聚体 VHH-Fc 融合体(homodimeric VHH-Fc fusions );
独立的多价(standalone multivalent/tandem VHHs)或串联VHH("beads-on-a-string"形式),包括双特异性构建体或结合人血清白蛋白(HSA)的构建体(bispecific, human serum albumin (HSA) binding construct);
CAR(嵌合抗原受体)细胞,其外结构域由串联组装的双表位VHH构成(......biparat opic VHHs assembled in tandem)。
图 3 展示了 VHH(蓝色)如何被应用于不同形式:作为 IgG 可变区、Fc 融合二聚体、可溶多价纳米抗体,或工程化细胞的抗原识别模块,其价态、特异性和半衰期通过连接肽、Fc 以及 HSA 结合体进行调控。这种架构上的多样性凸显了 VHH 的"即插即用"特性,以及它们与蛋白疗法和细胞疗法骨架的良好兼容性。
图 3|五种已获批的 VHH 基治疗药物所采用的结构架构。VHH 结构域以蓝色表示,其余组分以灰色表示。自左至右依次为:
Caplacizumab:一种单特异性、二价的串联 VHH 分子;
Netakimab:一种 IgG 样抗体,其中 VHH 替代了传统 VH,并与 VL 配对;
Envafolimab:一种 VHH–Fc 同源二聚体;
Ozoralizumab:一种三价"beads-on-a-string(串珠式)"构建体,两个抗TNF的 VHH分别位于两端,中间夹有一个结合人血清白蛋白(HSA)的VHH,用于延长体内半衰期;
Ciltacabtagene autoleucel:一种CAR-T细胞治疗产品,其嵌合抗原受体(CAR)的胞外结构域包含串联排列的双表位(biparatopic)抗 BCMA VHH。
这些分子形式充分展示了VHH作为模块化构件的优势:可通过连接肽、Fc融合、HSA 结合或细胞表面展示等方式,灵活调控分子的价态、特异性以及体内半衰期。
Caplacizumab
Caplacizumab(商品名 Cablivi),由 Ablynx(现为赛诺菲旗下公司)开发,于 2018 年首次在欧洲获批,用于治疗获得性血栓性血小板减少性紫癜(aTTP)(acquired thrombotic thrombocytopenic purpura)。该疾病是由血小板在超大冯·维尔布兰因子(vWF)多聚体上形成大规模聚集(large aggregates of platelets on ultralarge von Willebrand factor (vWF) multimers)所致,临床表现包括血小板减少(thrombocytopenia)、溶血性贫血(hemolytic anemia)、发热以及器官功能障碍(organdysfunction)。Caplacizumab 靶向vWF,抑制超大vWF与血小板之间的相互作用。从结构角度来看,该药物是 人源化抗 vWF 单特异性双价串联 VHH,由两个相同的抗原结合位点组成,中间由短的三丙氨酸(triple alanine)连接肽连接(见图 3)。
Netakimab
Netakimab(商品名 Efleira)由 Biocad 开发,于 2019 年在俄罗斯首次获批,用于治疗中重度斑块型银屑病(moderate-to-severe plaque psoriasis)。该人源化单克隆抗体能够中和白介素-17(IL-17),一种参与多种免疫相关疾病发病机制的细胞因子。从结构上看,Netakimab 是一种 改造型 IgG1,其中 VH 被抗 IL-17 的 VHH 替代,并与属于 VK3 家族的轻链配对(见图 3)。
Envafolimab
Envafolimab(商品名 Enweida)由 Alphamab Oncology 与 3D Medicines 共同开发,于 2021 年在中国获批,用于治疗微卫星不稳定性高(MSI-H)或错配修复缺陷(dMMR)的晚期实体瘤(microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) advanced solid tumors.)。作为一种 程序性细胞死亡配体 1(PD-L1)抑制剂,该分子属于免疫检查点抑制剂类别。Envafolimab 由 人源化的骆驼来源 VHH 构成,并与 IgG1 的铰链区(hinge)和 Fc 区融合(见图 3)。
Ozoralizumab
Ozoralizumab(商品名 Nanozora)于 2022 年在日本首次获批,用于 对现有治疗反应不足的类风湿关节炎(RA)患者(rheumatoid arthritis (RA) inadequately
managed by currently available treatment)。该化合物最初由Ablynx(赛诺菲子公司)开发,随后授权并由日本大正制药(Taisho Pharmaceuticals)进一步开发。Ozoralizumab 能够强效中和肿瘤坏死因子(TNF: tumor necrosis factor),一种多效性促炎细胞因子,在多种自身免疫疾病(如RA、银屑病或克罗恩病)的发病机制中发挥重要作用(a pleiotropic and proinflammatory cytokine playing a prominent role in the pathology of several autoimmune diseases, for instance, RA, psoriasis, or Crohn’s disease.)。从设计角度来看,Ozoralizumab 是一种三价双特异性抗体,由两个人源化抗TNF VHH 以及一个用于延长半衰期、结合人血清白蛋白(HSA)的人源化VHH组成,其串联顺序为VHH(TNF)–VHH(HSA)–VHH(TNF)(见图3)。各个构建模块之间通过两个九个氨基酸的柔性连接肽(Gly4SerGly3Ser)分隔。
Ciltacabtagene autoleucel
Ciltacabtagene autoleucel(商品名 CARVYKTI)于 2022 年在美国首次获批,用于 至少接受过四线治疗后复发/难治性多发性骨髓瘤的成年患者(relapsed/refractory multiple myeloma after at least four lines of therapy.)。Ciltacabtagene autoleucel 是由 Legend Biotech 与强生(Johnson & Johnson)共同开发的 CAR-T 细胞疗法。在治疗过程中,患者的 T 细胞被采集并在体外进行基因编辑,加入人工受体,使 T 细胞在识别抗原后能够被激活,随后再回输到患者体内。该疗法靶向 B 细胞成熟抗原(BCMA),该抗原优先在成熟B细胞上表达,其过度表达与多发性骨髓瘤相关。Ciltacabtagene autoleucel的CAR外结构域包含两个不同的(双表位)靶向 BCMA 的 VHH 结构域,串联排列并由柔性连接肽分隔(......arranged in tandem and separated by a flexible linker),从而实现高亲和力结合(见图 3)。CAR 构建体的信号部分包括 人 CD8α 铰链和跨膜区,随后是CD137(4-1BB)共刺激胞质区(costimulatory cytoplasmic domain),该胞质区与 人 CD3ζ 胞质区 融合。
临床 sdAbs 与 VHH 的序列特征
为了深入了解进入临床的sdAbs(包括 VHH)的特性,我们查询了TheraSAbDab(版本 19.02.2025),共识别出 46 个可变 sdAb 结构域。通过人工文献整理(Manual literature curation),又补充了 3 个 VHH 结构域(其中 2 个来自 ciltacabtagene autoleucel,1 个来自 netakimab),最终得到49个纳入临床或已上市疗法的(linical-stage or marketed therapeutics) sdAb 结构域。对于每个 sdAb,我们进行了 in silico 分析,包括:
序列聚类(基于 CDR3 及全长 sdAb)
人源相似性(最接近的人类 IGHV/IGHJ 匹配以及全可变区和框架区的身份百分比)(
closest human IGHV/IGHJ match and identity for full variable domain and framework region only)
非典型半胱氨酸的检测
CDR 和框架区潜在的 N-糖基化位点
计算全 sdAb 和 CDR 的等电点(pI)(见图 4)
结果显示,临床sdAbs的人源相似性中等偏高(与最近的人类种系基因相比,身份百分比为58.7–89.1%)。如预期,框架区的同源性通常高于全域同源性。值得注意的是,人源相似性最高的sdAbs来源于转基因动物平台,这些平台经过工程化处理可产生完全人源 sdAbs:
Porustobart的抗CTLA‑4 paratope 来源于转基因小鼠 HCAb 平台,可生成完全人源 HCAbs
Surovatamig的抗CD19 paratope 最初通过 Teneobio 的 UniRat 转基因大鼠平台发现,该平台可表达完全人源重链抗体(UniAbs)
________________________________________________________________
序列聚类显示,不同多特异性抗体中 sdAb 构建模块存在大量复用,或完全相同,或仅有少量序列差异。这种模块化特征(modularity)在HSA结合体中最为明显:Ozoralizumab、Sonelokimab、Vobarilizumab、Brivekimig、Lunsekimig、Isecarosmab、Gocatamig 和 Podentamig 中存在相同或高度相似的序列,这反映了一种通过结合内源性HSA并利用新生儿Fc受体(FcRn)回收来延长体内暴露、降低肾清除的常用策略。( reflecting a common strategy to prolong exposure by
engaging endogenous HSA and leveraging neonatal Fc receptor (FcRn) recycling to reduce renal clearance.)
同样,在 Envafolimab 和 Erfonrilimab 中发现完全相同的抗 PD-L1 paratopes,凸显了(underscoring)经过验证的sdAbs作为可互换组件(interchangeable components)在不同药物发现和开发项目中应用的价值。
最常见的靶点类别包括:
HSA(延长半衰期)
免疫检查点(PD-L1、CTLA-4)
细胞因子(TNFα、IL-17A/F、IL-13)
值得注意的是,49个sdAbs中有6个携带额外的二硫键,将CDR3与CDR1(IMGT 38)或 FR2(IMGT 50 或 55)中的半胱氨酸连接。如一般架构部分(As outlined in the general architecture section)及图 1(G)和 1(H) 所示,这些连接位点在不同物种中呈富集状态,有助于稳定和塑造 CDR3 环。
临床 sdAbs 中 CDR 和框架区均未发现 N‑糖基化位点(N‑X‑S/T)( Notably, no N‑glycosylation motifs (N‑X‑S/T)are present in either CDRs or frameworks in this clinical set.)。此外,临床 sdAbs 常呈碱性:49个sdAbs中34 个(≈69%)的 VHH 等电点 >7.5(图 4 蓝色标记)。
FR2的hallmark motifs主要由FERF(15/49,30.6%) 和 VGLW(12/49,24.5%) 构成,其余 22 个 motif 分布在多样的序列中(如 FERG、FERR、FGLG、YQRL/YQRW、YERL、VGPW)。
图 4|临床阶段及已上市 sdAb(n = 49)的序列特征。序列来源于 TheraSAbDab(版本 19.02.2025)。采用 IMGT 编号体系进行区域划分(region delineation),并用于 FR2 标志性位点(hallmark positions)的定义。
"CDR3 (85% id)"和 "VHH (100% id)" 分别表示在 CDR3 区域 85% 序列一致性以及 全长 sdAb 100% 序列一致性条件下分配的聚类编号;数值即为聚类 ID,不同治疗分子中出现相同 ID 表明完全相同的 VHH 序列或高度相似(聚类)的 CDR3 序列被重复使用。( the numeric entry is the cluster id, and repeated IDs across therapeutics indicate re‑use of identical (full VHH) or clustered (CDR3) sequences. )
"Most similar germline" 列出与之最接近的人源 IGHV/IGHJ 胚系基因对;"SEQ-ID VHH"和 "SEQ-ID fw"分别给出全长可变区以及仅框架区(IMGT FR1–FR4)的序列一致性百分比。
PTMs 表示翻译后修饰,其中
"non-standard Cys"指预测是否存在除保守的域内二硫键半胱氨酸之外的额外半胱氨酸(存在为 2,不存在为 0);
"N-GLYCOSYLATION" 表示在所分析的所有 sdAb 中(all sdAbs scrutinized)均不存在经典的 N-X-S/T 糖基化基序(X ≠ 脯氨酸)。
等电点 "pI VHH" 和 "pI CDR" 分别基于全长 VHH以及所有 CDR 合并区域计算;当 pI > 7.5 时以蓝色标注,否则以浅红色标注。
"hm" 列出了位于 IMGT 位点 42、49、50 和 52 的 FR2 标志性基序。
利用骆驼科来源 sdAbs 的抗体工程
由于VHH结构域不与轻链配对,因此可独立发挥抗原结合功能(autonomous
paratope),这类sdAbs可以方便地整合到前所未有多样化的抗体架构中(an unprecedented diversity of Ab architectures),包括多特异性或多价设计(见图 5(A))。这一特性在所有五种已上市的含VHH的疗法中(VHH-harboring therapeutics)得到了体现,它们采用了不同的抗体格式(见图 3,如上所述)。研究表明,抗体格式、本体paratope的价数(ultimately paratope valencies)以及各个抗原结合位点在整体架构中的空间取向,都会显著影响功能表现。在这方面,VHH提供了(afford) "即插即用"式的优势,使得研究者能够方便地生成和测试不同的抗体格式,从而筛选出符合特定作用机制的(fulfill a prescribed mode-of-action)最佳设计。
图 5|利用 VHH 作为构建模块的抗体设计示例。
(A) 采用“串珠式(beads-on-a-string)”的串联设计架构,可将不同的表位结合价数(valency)和特异性便捷地整合到同一分子中;此外,还可通过该方式整合细胞因子等其他功能性负载。(Tandem design architectures in a beads-on-a-string manner enable the facile incorporation of different paratope valencies and specificities into a given molecule. Also,other payloads such as cytokines can be integrated in this manner.)
(B) 由于缺乏轻链,VHH 可通过肽连接子轻松融合至已有的 IgG 上,从而产生双特异性。( Due to the absence of a light chain, VHHs can easily be fused to a pre-existing IgG via a peptide linker to generate bispecificity.)
(C) 采用重链异源二聚化技术,可构建具有不同价数的、基于 VHH 的 IgG 样双特异或多特异抗体。(The use of a heavy chain heterodimerization technique allows for the generation of bi- and multispecific VHH-based IgG-like bi- and multispecifics with varying valencies.)
(D) 为实现半衰期延长,VHH 可与 IgG Fc 区或人血清白蛋白(HSA)结合分子进行融合。( For half-life extension, VHHs can either be fused to an IgG Fc region or to an HSA binder. Figure generated with bioRender (www.biorender.com).)
________________________________________________________________
VHH 可以 轻松与已存在且特性明确的 paratope 结合,用于构建双功能甚至多功能抗体。为此,可以将 sdAb paratope(或多个不同 paratope)通过 柔性连接肽 直接融合到母抗体的自由 N 端或 C 端,从而生成 双特异性抗体(bsAb),实现对两个 paratope 的双价靶向(见图 5(B))。
________________________________________________________________
如果需要单价结合其中一个或两个paratope,则可采用重链异源二聚化技术,例如 knob-into-hole(KiH) 或 strand-exchange engineered domain 技术(SEED)(见图 5(C))。一个重要考虑因素是:Fab 构建的经典 VH 结构域和 VHH 结构域的 N 端通常位于 CDR3 附近(both classical VH domains within Fab-based paratopes and VHH domains have their N-terminus positioned near CDR3),而 CDR3 往往是抗原结合最关键的区域。因此,在多价或多特异性融合中,VHH 的方向和位置可能显著影响结合能力,例如通过空间阻碍(steric hindrance),有些构建体表现出对 N 端或 C 端位置的明显偏好。这种位置效应可能影响 VHH 放置在其他蛋白结构 C 端时的 paratope 可及性(accessibility),而合理的连接肽设计可以减轻不佳定位带来的影响。(......appropriate linker design can help mitigate suboptimal positioning effects.)
________________________________________________________________
仅由 sdAb 构成的分子通常显示半衰期较短,需要频繁给药(requiring frequent administration into patients)。为延长 VHH 的半衰期,可将 sdAb 基因融合至 IgG Fc 结构域,通过 FcRn 循环实现半衰期延长(图 5(D) 左)。该策略已应用于 Envafolimab 的工程设计,其皮下注射给药(which is administered subcutaneously),首剂半衰期为 14 天,稳态半衰期为 23 天。另一种常用策略是将治疗性 VHH “载荷"融合到 针对 HSA 的 sdAb 上(为了实现良好的药代动力学(favorable pharmacokinetics)),通过类似 IgG Fc 融合的方式,利用 FcRn 延长半衰期(图 5(D) 右)。例如 Ozoralizumab,一种双价 TNF 阻断 VHH 治疗剂,融合了 HSA 定向 sdAb,皮下注射给药,半衰期约为 18 天。实际上,近期在临床试验中评估的多种基于 VHH 的双特异性分子都集成了上述半衰期延长策略之一。
未来展望
基于 VHH 的生物制剂治疗领域仍在快速扩展。尽管第一波临床 VHH 衍生分子主要集中于阻断剂(clinical VHH-derived molecules mainly encompassed blockers)——包括针对可溶性疾病介质(soluble disease mediators)或膜结合受体的阻断剂(membrane-bound receptors),以及针对肿瘤相关抗原(TAA)的"结合臂",但该领域显然已经超越了目前五种获批疗法,新的作用模式正在出现(he field has clearly matured beyond the five currently approved therapeutics, with novel modes of action on the horizon.)。在这方面,基于多价 VHH 的激动剂,针对 TNF 受体超家族成员,已经进入临床开发阶段。例如,Ozekibart 是一种四价 (VHH–VHH)-Fc 融合蛋白,可靶向并聚集死亡受体 5(DR5),从而产生强烈的 DR5 激动作用,最终引发肿瘤细胞凋亡(tumor cell apoptosis)。此外,INBRX-106 是一种六价 (VHH-VHH-VHH)-Fc 抗体衍生物(derivative),可靶向并激活(agonizes)OX40,这是一种对 T 细胞存活和分化(differentiation)非常重要的共刺激受体(costimulatory receptor)。更进一步,VHH 正越来越多地被纳入 下一代治疗方式(Beyond, VHHs are increasingly being incorporated into next-generation treatment modalitie)。这包括但不限于:
抗体-药物偶联物(ADCs),其中 VHH 被认为能够增强肿瘤穿透性(penetration and ultimately),从而实现有效的药物递送(payload delivery);
CAR-T 细胞疗法,利用多功能 VHH 构建的靶向受体,其中 Ciltacabtagene autoleucel 是首个获批的基于 VHH 的 CAR-T 细胞疗法。
在接下来的章节中,我们将简要讨论一些由 sdAbs 驱动的新兴治疗作用机制。(
some emerging therapeutic mechanisms of action that are mediated by
sdAbs.)
VHH 作为效应细胞重定向的构建模块
VHH(以及 sdAbs 整体)是进行效应细胞重定向的重要构建模块(valuable building blocks)。例如,已有 VHH 被用于通过双特异性方式同时靶向 γδ T 细胞受体 和 肿瘤相关抗原(TAA)来重定向并激活 γδ T 细胞。这类 γδ T 细胞激活剂已被开发用于多种肿瘤适应症,从血液系统恶性肿瘤(hematologic malignancies)到实体瘤(solid tumors),靶点包括 CD1d、CD33、CD123 或 EGFR。此外,还已有 VHH 被开发用于靶向 CD3,以构建传统的 T 细胞激活剂。除了 T 细胞重定向,VHH 也被用于构建 自然杀伤(NK)细胞激活剂(the construction of natural killer (NK) cell engagers.)。典型示例(Prominent examples)包括(下一代)TriKEs(三特异性杀伤激活分子)(Tri-specific Killer Engager molecules),其基于三部分:
一个靶向 CD16 的 VHH,用于 NK 细胞重定向;
一个 IL-15 模块(moiety);
一个特异性 TAA 的结合位点,可为 单链可变片段(scFv) 或 VHH。
此外,针对自然细胞毒性(Cytotoxicity)受体 NKp30 和 NKp46 的 VHH 已被用于构建高效的 NK 细胞激活剂。研究显示,单个结合位点的空间方向以及结合位点的价数对肿瘤细胞杀伤效率具有显著影响。(the spatial orientation of individual paratopes as well as paratope valencies significantly impact tumor cell killing efficiencies.)
VHH 作为细胞因子模拟物(cytokine mimetics)
细胞因子通常是分泌型信号蛋白(secreted signaling proteins ),在调控炎症反应(regulating inflammation)、免疫应答、细胞生长、组织修复以及细胞凋亡(apoptosis)等过程中发挥关键作用。其强大的免疫调节(immunomodulatory)特性已促成多种细胞因子药物获批(approval of several cytokines),用于治疗癌症、多发性硬化(multiple sclerosis)、贫血(anemia)、中性粒细胞减少症(neutropenia)或血小板减少症(thrombocytopenia)等疾病。然而,细胞因子的治疗应用受到多方面限制,包括多效性(pleiotropic)且依赖于生理环境(context-dependent effect)的作用方式、体内半衰期短,以及全身给药时生物分布不理想(suboptimal biodistribution when administered systemically)。此外,剂量限制性毒性(dose-limiting toxicities)也可能出现,这在一定程度上源于细胞因子级联反应的非特异性启动(the initiation of cytokine cascades)。
除了直接对细胞因子本身进行工程改造之外,另一种用于精细调控特定生物学功能的策略是构建细胞因子模拟物(cytokine mimetics),也称为替代性激动剂(surrogate agonists)。在这一策略中,通常利用双特异性或多特异性 sdAb靶向某一(多为异源二聚体的)细胞因子受体,从而诱导受体激活并产生激动效应(trigger receptor agonism)。通过这种方式,可以对细胞因子的功能进行高度调控,例如信号强度或细胞亚群偏向性(in terms of signaling strength or cell subset bias)。为此,可以在双特异性或多特异性构型中筛选针对受体不同亚基的多种表位组合,从而诱导形成不同的受体几何构象(inducing distinct receptor geometries),最终导致下游信号通路的差异化激活(resulting in differential downstream signaling)。此外,使用 VHH 或更广义的 sdAb 还允许在设计中灵活调控表位结合价数(valency)以及各个表位在整体分子架构中的空间取向,以进一步精细调节功能效应。基于 sdAb 的细胞因子模拟物已被报道可用于多种细胞因子体系,例如 IL-2、IL-10、IL-12、IL-18 以及 I 型干扰素(interferons)。此外,还开发了人工细胞因子受体激动剂以及具有条件性活性的替代性激动剂,充分凸显了sdAb在定制和精细塑造细胞因子生物学(tailor-make cytokine biology)功能方面所具备的巨大工程化潜力。(......clearly emphasizing the plethora of engineering options of sdAbs to tailor-make cytokine biology.)
VHH 作为变构调节因子(allosteric modulators)
变构调节(Allostery)是蛋白质调控中的一种基本机制,其通过在远离活性位点的位置发生的构象和动力学变化来调节蛋白活性(modulation of activity)。传统上,变构调节主要在小分子药物领域中得到研究和应用;然而,近年来,抗体,尤其是 VHH,正逐渐显现为强有力的变构调节工具(allosteric modulators.)。通过结合不同于天然配体结合位点的表位,VHH能够重塑靶蛋白的构象景观图(conformational landscape),从而产生区别于传统抑制剂的治疗学效应特征(therapeutic profile)。________________________________________________________________
这一潜力在表皮生长因子受体(EGFR)(Epidermal growth factor receptor)相关研究中得到了充分体现。研究人员发现,一类变构型VHH并非通过阻断配体结合,而是通过稳定信号失活(signal-incompetent)的受体构象来抑制EGFR活性。通过将结构学与功能学实验相结合,并辅以变构通讯(allosteric communication)的计算模型分析,研究揭示了抗体结合如何扰动受体的远端区域(perturbs distal regions of the receptor),从而实现功能调控。这些综合性研究(These combined approache)展示了实验方法与计算手段如何相互印证,并最终用于理性化解释并指导变构抗体的设计。(……methods can converge to rationalize and ultimately guide the design of allosteric antibodies.)
在另一靶点体系中,Li 及其同事报道了作用于 α7 型烟碱型乙酰胆碱受体(α7 nicotinic acetylcholine receptor)的 VHH,其表现为沉默型(silent)或正向变构调节因子(positive allosteric modulators)。更为重要的是,VHH 介导的变构调节已经进入转化神经科学领域(translational neuroscience):近期一项研究表明,一种作为代谢型谷氨酸受体mGlu2(the metabotropic glutamate receptor mGlu2)的正向变构调节因子的VHH,能够挽救与NMDA受体功能低下相关的行为缺陷(rescued behavioral deficits associated with NMDA receptor hypofunction),该模型被广泛用于研究精神分裂症中的认知障碍(cognitive impairment in schizophrenia)。
________________________________________________________________
除了在治疗领域的应用潜力之外,VHH也已成为结构生物学中不可或缺的(indispensable)变构研究工具。Steyaert 及其同事率先将 VHH 用于稳定 G 蛋白偶联受体(GPCR)的特定构象状态,从而获得了β₂-肾上腺素能受体(β2-adrenergic receptor)与G蛋白复合物的里程碑式(landmark)结构。
在此基础上,Manglik 等人开发了 Nb80、Nb60 等 VHH,这些分子能够捕获(trap) β₂-肾上腺素能受体的不同构象状态,并揭示了激动剂效能(agonist efficacy)背后的分子机制。
Scheerer 团队也提供了更多重要实例,进一步推动了 GPCR 结构生物学的发展。例如,在解析黑皮质素-4 受体(MC4R)与异源三聚体刺激型 G 蛋白 Gs 复合物的活化态结构时(the melanocortin-4 receptor in complex with the heterotrimeric
stimulatory G protein Gs),一个起稳定作用的 VHH(Nb35)对于捕获受体–G 蛋白装配体并实现高分辨率冷冻电镜(cryo-EM)结构解析至关重要。
________________________________________________________________
综合来看,这些进展确立了 VHH 作为多功能变构调节因子(versatile allosteric modulators:)的重要地位:一方面,它们是能够精细调控蛋白活性的治疗性分子;另一方面,它们也是揭示复杂信号蛋白动态本质的强有力研究工具。
口服递送及替代给药途径
由于其内在的理化稳定性(intrinsic physicochemical stability),VHH 在针对人类和动物胃肠道(GI)病原体(gastrointestinal (GI) pathogens)的口服给药方面具有潜在吸引力。为此,研究者提出了多种策略,以进一步提高 VHH 对极端 pH、热和蛋白水解作用(proteolysis)的耐受性(resistance),并通过针对结合价数(avidity)和靶标覆盖度优化的分子构型,增强其在胃和肠道环境中(gastric and intestinal environment)的功能表现。在这一背景下(In this regard),多种多价构型已被报道,例如双价VHH–VHH 构建体、Fc/分泌型 IgA 融合蛋白(secretory IgA fusions),以及合成的五聚体 VHH–verotoxin B 亚基融合蛋白(synthetic pentameric VHH-verotoxin subunit B fusions)。这些分子在动物模型中表现出增强的病原体凝集能力(pathogen agglutination),从而改善了对弯曲杆菌(Campylobacter)、产志贺毒素的大肠杆菌(STEC)(Shiga toxin-producing Escherichia coli)及相关病原体的控制效果。
________________________________________________________________
为在通过胃肠道( the GI tract)后仍保持蛋白功能,Arbabi-Ghahroudi 及其同事通过二硫键工程化并结合在胃肠道蛋白酶存在条件下对易错 PCR 文库进行筛选的方法(
a panning approach of an error-prone polymerase-chain reaction library in the presence of GI proteases.),获得了耐蛋白酶的 VHH(protease-resistant VHHs),能够抑制 Campylobacter jejuni 的运动性(motility)。
除了降低细菌感染风险之外,口服给药的VHH(orally administered VHHs)也已被用于评估其在中和胃肠道病毒感染以及自身免疫相关胃肠疾病中的潜力。例如,一种针对轮状病毒衣壳蛋白(a capsid protein ofrotavirus )的 VHH 在仔猪piglets中显示出对腹泻diarrhea的保护作用,并在婴儿中显著减少了粪便排出量(stool output)。
此外,Ota 及其同事报道了一种经工程化改造、具有蛋白酶稳定性的 VHH,可靶向 IL-23 受体(IL-23R)用于治疗炎症性肠病(flammatory bowel diseases)。该分子在小鼠模型(in murine models)中表现出有效的信号通路抑制作用,并在非人灵长类动物口服给药后(non-human primates following oral administration),在循环系统中维持了持续的 IL-23R 抑制效果。
________________________________________________________________
尽管已有许多令人鼓舞的研究实例,口服给药的抗体类治疗分子在体内维持稳定性仍然是一个主要障碍( a major obstacle)。因此,人们开始探索替代性的递送途径(alternative delivery routes)。其中一种颇具吸引力的策略是,利用被归类为**“普遍认为安全(GRAS)”的生物体(organisms)在体内原位递送(in situ delivery ) VHH,例如 乳酸杆菌/乳酸乳球菌(Lactobacillus/Lactococcus)菌株、蓝藻Arthrospira platensis(螺旋藻)(cyanobacterium Arthrospira platensis (spirulina)),以及植物宿主系统。在这一方面,Tokuhara等人表明,通过转基因水稻递送多聚化的抗轮状病毒 VHH(mice receiving genetically modified rice delivering multimeric anti‑rotavirus VHHs),即使在储存超过一年并在给药前经受煮沸处理后(boiling prior to administration),仍能在小鼠模型中对轮状病毒感染提供有效的保护作用(efficacious protection )。
________________________________________________________________
尽管在VHH的口服应用(oral application)及替代递送方式(alternative delivery methods)方面已经取得了显著进展(substantial progres),但其成功落地仍将取决于多个关键因素,包括:胃肠道内精确的给药与释放控制(precise GI dosing and release)、可规模化且低成本的生产工艺(scalable low‑cost manufacturing)、更高稳定性的制剂开发(stability formulation),以及针对含转基因生物(GMO)产品的清晰监管路径(clear regulatory pathway)。
细胞疗法抗体药物偶联物免疫疗法引进/卖出
2026-01-08
·科佰生物
01
背景
白细胞介素17(interleukin17,IL17)是目前已发现的30余种白细胞介素之一,按序号排在第17位。IL17由CD4T细胞分泌,能够诱导上皮细胞、内皮细胞、成纤维细胞合成分泌IL-6、IL-8、G-CSF、PGE2,促进ICAM-1的表达。白细胞介素 - 17 家族包含6 个成员的配体(IL-17A~IL-17F,其中IL-17E又称为IL-25)和5个受体(IL-17RA~IL-17RD和SEF)是关键的细胞因子群体,其展现出广泛的生物学功能,包括调节多种自身免疫性疾病和炎症性疾病中的炎症反应过程,例如多发性硬化症、视神经炎谱系疾病、重症肌无力、吉兰 - 巴雷综合征、急性播散性脑脊髓炎、糖尿病、炎症性皮肤病、关节炎症以及癌症。
IL-17家族的成员都具有相似的蛋白质结构,其中研究最多的是IL-17A和IL-17F。IL-17A 作为该家族的典型成员,它刚刚迎来了发现后的第 27 个年头。IL-17A(因其在自身免疫性疾病中的促炎作用而备受关注,且已有数种针对白细胞介素 - 17A 的单克隆抗体在临床实践中得到成功应用。然而,在过去十年中,人们逐渐认识到 IL-17 的功能远比简单地引发炎症更为复杂。越来越多的证据表明,IL-17 在应对损伤、生理应激和感染时,在维持健康方面具有重要的环境和组织依赖性作用。
IL17的功能
IL-17 细胞因子具有一个半胱氨酸环结构,它们会与特定的 IL-17R 受体结合,通过 SEFIR、SEFEX 和 CBAD 结构域激活免疫信号传导。IL-17 信号传导始于 IL-17A/A、IL-17A/F 或 IL-17F/F 细胞因子与其受体(IL-17RA 和 IL-17RC)的结合,或者 IL-17E/E 细胞因子与其受体(IL-17RA 和 IL-17RB)的结合。当配体结合后,Act1 会激活多种独立的信号传导途径,这些途径通过不同的 TRAF 蛋白介导。TRAF6 的激活会导致 NF-κB、C/EBPβ、C/EBPδ 和 MAPK 信号通路的触发。IL-17R-Act1 复合物还通过 TRAF4 与 MEKK3 和 MEK5 结合,从而激活 ERK5。不同类别的抑制剂,如泛素酶(TRAF3)、去泛素酶(A20)、RBP(HuR、ACT1、Aridα 和 DDX3X)、内切核糖核酸酶(MCPIP1/Regnase-1)和微小 RNA(miR-23b),通过各种独立的机制负向调节 IL-17 信号传导。IL-17C 主要由上皮细胞表达。当 IL-17RA/RE 受体复合物表达时,上皮细胞本身和 TH17 细胞都是 IL-17C 的作用靶点。除了增加 Th17 细胞中 IL17A 的表达外,IL-17C 还通过间接方式增强吸引中性粒细胞的趋化因子在上皮细胞中的表达,最终导致强烈的炎症反应。
IL-17 细胞因子参与多种免疫调节,对自身免疫性疾病及免疫相关疾病(如多发性硬化症、视神经脊髓炎谱系疾病、重症肌无力、吉兰-巴雷综合征和急性播散性脑脊髓炎)以及非神经免疫性疾病中的炎症和病理过程产生影响。
IL17的细胞模型
作为自免赛道的“全能选手”,目前国内外已上市的靶向IL-17家族的自免药物有6款 (优时比的bimekizumab 、诺华Secukinumab、礼来Ixekizumab、Biocad的netakimab、安进和阿斯利康开发的brodalumab以及江苏恒瑞医药的Vunakizumab(安达静)。其中诺华的Secukinumab(司库奇优)作为首个获批上市的IL-17药,其2020年销售额突破40亿美元),涉及的适应症包括银屑病、银屑病关节炎、强直性脊柱炎等,与此同时,这些药物正通过临床试验向炎症性肠病(IBD)、多发性硬化症(MS)等新领域拓展。在研发端,IL-17靶点热度持续攀升——超20款在研药物(含双抗、小分子抑制剂等)处于临床阶段。
部分在研药物进展如下:
为了助力IL17相关靶点药物的研发,科佰生物分别开发了针对IL17A/F和IL25的细胞模型,用于候选药物早期机理研究。部分结果如下:
IL17A/17F Effector Reporter Cell CBP74484
Figure 4. Dose Response of Ligands in IL17A/17F Effector Reporter Cell (C45).
Figure 5. Inhibition of Human IL17F induced Reporter Activity by IL17RA Blocking or IL17F Neutralization Ab in IL17A/17F Effector Reporter Cell (C45).
IL25 Effector Reporter Cell(Suspension) CBP74480
Figure 6. Inhibition of Human IL25-induced Reporter Activity by IL25 Neutralization Ab or IL17RA&RB Blocking Abs in IL25 Effector Reporter Cell (Suspension, C9).
药物靶点模型
报告基因细胞模型可以很好的反映分子作用机制,同时具备更小的变异性和更好的可操作性,已被中检院及药企广泛应用于抗体药物生物活性的检定,对于药物研发、质量控制、批次放行都有重要意义。
科佰生物公司十分重视研发创新,凭借细胞功能改造技术、高精度和灵活的基因编辑工具平台,提供包括激酶,GPCR,免疫治疗,耐药等多类疾病靶点的药物检测细胞模型。目前已覆盖1500多株现货细胞模型,同时提供高质量的Cell-base生物测活服务。
免疫治疗靶点细胞模型
● T Cells Activation Assays (NFAT, IL2, NFκB….)
● Fc Effectors Activity Assays ( ADCC, ADCPs…)
● Immune Checkpoint Bioassays: Co-Inhibitory Targets (PD-1/PD-L1&2, TIGIT/CD155, CTLA4, LAG3, LILRB4/APOE, CD112R/CD112, SIRPα/CD47, TIM-3, BTLA/HVEM, CD161/CLEC2D, TIGIT&PD-1, LAG3&PD-1, CTLA4&PD-1 Combi…)
● Immune Checkpoint Bioassays: Co-Stimulatory Targets (OX40, 4-1BB, GITR, CD27, HVEM/LIGHT, CD28, BTLA…)
● Cytokines and Growth Factor Assays ( BCMA, TGFβ, EGF, CSF1R, IL2, IL15, IL4&13, IL6, IL10, IL11, IL12, IL18, IL23, IL31, IL36, IFNs, OSMR, RANKL, TPO, TIE2, Wnt, EPO, VEGF, TSLP, NGF…)
● Others (TLR family members, STING,A2A family members, SARS Cov2…)
-科佰生物产品-
免疫治疗细胞库
点击查看
BaF3激酶靶点细胞株
点击查看
GPCR细胞库
点击查看
耐药细胞
点击查看
<< 滑动查看下一张图片 >>
部分文字,图片来源网络,如涉及侵权,请联系告知。
●GARP/LTGF-β细胞模型
●免疫检查重要靶点CTLA4
●免疫检查点靶点——LILRB细胞模型
关注科佰生物
了解更多资讯
热线电话:4008-750-250
药靶模型联系方式:华东销售经理(上海):18240630236华东销售经理(上海、江苏、安徽):15715191010华中&华西销售经理:18071545918华中&西南销售经理:13871580511华北销售经理:18628311252
华南销售经理:13823536064
全国销售经理:13816461235
邮箱:sales@cobioer.com
网站:www.cobioer.com
临床研究申请上市
2026-01-07
·科学战银
点击上面文字添加关注!推荐指数★★★★★
【伊顿健康导读】
如果你是正在被中重度银屑病困扰的患者,可能正面临着选择困难:老牌药效不够、进口药价格昂贵、打针麻烦……而最近,国家药监局受理、批准了一大批国产新药的消息,让注射类生物制剂突然热闹非凡。是等待更新、更多的选择,还是现在就行动?这波新浪潮,到底会给治疗带来哪些实质性改变?本文将用真实数据和临床进展,帮你理清头绪。
IL-17抑制剂
1.莱康奇塔单抗(LZM012)是丽珠医药公布的首款申报上市的IL-17A/F双靶点抑制剂
III期头对头研究结果显示,其治疗中重度斑块型银屑病疗效显著。与司库奇尤单抗(可善挺)相比,莱康奇塔单抗起效更快(第4周PASI 75应答率65.7% vs 50.3%),第12周PASI 100应答率更高(49.5% vs 40.2%),且长期疗效更优(第52周PASI 100应答率75.9% vs 61.6%)。其安全性良好,不良事件发生率与对照组相当。
2.偌考奇拜单抗(JS005)注射液是君实生物自主研发的特异性抗IL-17A单克隆抗体
一项多中心临床研究共入组747例中重度银屑病患者。数据显示,在III期研究中,使用偌考奇拜单抗治疗12周后,患者PASI 75/90/100及sPGA 0/1应答率均显著优于安慰剂组。疗效在长达52周的治疗期内保持稳定,且总体安全性良好。
3.古莫奇单抗(AK111)是康方生物自主研发的靶向IL-17A单克隆抗体
52周PASI 90率接近90%,PASI 100率提升至接近65%。已公布的数据显示,这些国产新药的不良事件发生率与对照组相当或略低,常见不良反应类型与已知IL-17抑制剂类似,未出现新的重大安全信号,总体耐受性良好。
4.KH917注射液是康弘药业自研的IL-17A生物类似药
安全性与有效性理论上应与原研药拓咨®(依奇珠单抗)一致。临床数据显示:用于中重度斑块型银屑病时,第12周PASI 75(银屑病面积和严重程度指数改善75%)率可达80%以上,PASI 90率可达50%以上;常见不良反应为注射部位反应(如红斑、瘙痒)、上呼吸道感染、头痛,多数为轻至中度,严重不良反应发生率低(如感染、过敏反应)。
5.GLR1023注射液是甘李药业的IL-17生物类似药
安全性和有效性需与原研药司库奇尤单抗高度相似(根据《生物类似药研发与评价技术指导原则》)。在III期临床试验中,第12周PASI 75应答率(银屑病面积与严重程度指数改善≥75%)约为80%-90%,PASI 100应答率(完全清除)约为30%-40%;常见不良事件(AE)为上呼吸道感染、鼻咽炎、头痛等,多为轻度至中度,严重不良事件(SAE)发生率极低(<1%)。GLR1023作为生物类似药,预期安全性和有效性与司库奇尤单抗一致,但需等待I期及后续临床试验结果验证。
6.Netakimab(尼塔奇单抗)是由俄罗斯Biocad公司研发的一款IL-17A单克隆抗体
该药物于2019年5月在俄罗斯获批,随后于2020年8月在白俄罗斯获准用于治疗中重度斑块状银屑病、银屑病关节炎及强直性脊柱炎。公布的临床数据显示,治疗第12周时,有85%的患者达到PASI 75(皮损显著改善),34%的患者实现PASI 100(皮损完全清除)。
7.BAT2306是百奥泰生物制药的司库奇尤单抗(可善挺®)的生物类似药
其通过特异性结合IL-17A,阻断其与受体结合,从而抑制下游促炎因子释放。IL-17A是驱动银屑病、银屑病关节炎及强直性脊柱炎等自身免疫疾病的关键炎症因子,患者体内其水平通常显著升高。
8.三生国健的608(IL-17A单抗)
研发进展顺利,其治疗成人中重度斑块状银屑病的适应症已于2024年第四季度提交上市申请,临床数据显示疗效全面,关键指标优于同类产品,且复发率低。治疗强直性脊柱炎的适应症已进入III期临床,II期结果积极。
9.巨石生物开发的司库奇尤单抗生物类似药(IL-17A单抗)
一项验证SYS6012与可善挺®(司库奇尤单抗)治疗中重度斑块状银屑病疗效等效性的关键Ⅲ期研究公布数据。患者按1:1比例随机分组,主要终点为第12周PASI 75应答率。研究已达到主要终点,统计分析证实SYS6012与可善挺具有临床等效性。同时,SYS6012表现出良好的安全性,未出现新的或非预期的安全信号。
10.CMAB015是迈博药业生物类似药(IL-17A单抗)
对于中重度慢性斑块状银屑病患者,CMAB015临床试验完成入组带来了新的希望。该药物有望在近期为患者提供一种更具疗效和安全性的治疗新选择。相较于传统疗法,CMAB015凭借其创新作用机制,或能更有效地控制疾病进展,降低复发风险。
脓疱型银屑病(IL-36)-3款药物可选择
1.AnaptysBio公司开发的Imsidolimab注射液(IL-36R)
基于公开的临床试验结果:泛发性脓疱型银屑病(GPP)关键III期试验(GEMINI-1),单次静脉注射750mg后第4周,53.3%的患者达到皮肤"清除或几乎清除"(GPPPGA 0/1),显著优于安慰剂组的13.3%(p=0.0131)。持续应答疗效可持续至第12周,脓疱和红斑明显消退。部分患者在给药后第8天脓疱改善率达80%,第29天皮肤清除率提升至94%。总体耐受性良好,在GPP试验中,未报告严重不良事件(SAE),常见不良事件为轻度至中度感染,发生率与安慰剂组相当。
2.由勃林格殷格翰创新研发、利奥制药收购交割的佩索利单抗(IL-36R)
在临床研究中,研究者进一步探索了佩索利单抗(圣利卓)预防脓疱型银屑病发作的最佳方案。数据显示,采用300mg q12w(每12周一次)皮下注射方案的患者中,分别有29.0%(Effisayil 2)和33.3%(Effisayil ON)出现病情发作或需调整给药方案。结果表明该给药间隔在长期预防中可能存在局限性。
3.华奥泰的瑞西奇拜单抗(IL-36R)
在关键III期临床研究被证实,瑞西奇拜单抗治疗泛发性脓疱型银屑病(GPP)疗效显著。单次静脉给药后第一周即可快速清除皮肤脓疱,显著优于安慰剂,达到所有主要及次要终点。该药起效迅速,对控制GPP急性发作具有重要临床价值,且安全性良好,未发现新的非预期风险。
干细胞疗法:
华夏源细胞工程集团研发的ELPIS人脐带间充质干细胞注射液
临床数据、安全性和疗效的综合分析,安全性数据整体安全性良好,在中重度斑块型银屑病的I期临床试验(44例受试者)中,仅报告1例轻微不良反应(短暂性低热),未发现严重不良事件或免疫排斥反应。银屑病I期临床中,患者银屑病面积与严重程度指数(PASI)平均改善≥50%,部分患者皮损完全消退。
总结
巨大的临床需求和市场空间,驱动了国内药企的集中研发。从生物类似药(仿制已上市产品)到创新单抗(甚至双靶点),再到给药方式优化,企业们在“疗效、安全、便捷、可及”四个维度上竞速,目的只有一个:让更多中国患者用上更好、更可负担的先进治疗。这意味着,患者的选择权和议价空间,正在快速变大。
这些药物在起效速度、皮损清除深度和长期维持上,都展现了不逊于甚至在某些指标上优于现有治疗的实力,为患者提供了经科学验证的有效新选择。
临床招募分享
神州细胞针对中重度斑块状银屑病患者 SCT650C 的Ⅲ期临床试验研究项目正在进行中。招募年龄≥18岁的伴或不伴有银屑病关节炎的中重度斑块状银屑病患者。
药物信息
药物名称:SCT650C注射液
剂型:注射剂
用法:皮下注射
作用机制:重组抗IL-17A单克隆抗体,通过高亲和力结合IL-17A蛋白,阻断其与受体IL-17RA的结合,抑制炎症反应,减轻银屑病皮肤症状。
此外还有目前正在开展的银屑病的匹康奇拜单抗(已上市)多项临床研究:
①针对银屑病关节炎的长期治疗策略研究
②针对青少年银屑病III期临床研究
不排斥口服药物患者也可同步报名。目前多项口服新药临床研究正在开展中,无需注射,用药更为方便。如您对口服治疗方式感兴趣,或有相关治疗需求,欢迎进一步咨询与评估报名。
ICP-332 II期口服的TYK2抑制剂针对中重度斑块型银屑病,一共是12周的用药周期。
符合条件、用药、体检由申办方承担,不收取费用,同时会有可观的交通补贴和营养补贴。
有需要的患者可以报名
了解更多项目详情
想了解更多银屑病问题
可以添加工作人员
临床试验是什么?
临床试验是新药获批上市前必需的科学验证环节(紧急授权等特殊情况除外)。申办方(通常为制药企业)需向国家药品监督管理部门提交申请,获得批准后,方可在具备国家药物临床试验机构资质的三甲医院内实施。
试验全程受到国家监管部门及医院伦理委员会的双重监督,以充分保障受试者的安全与权益。
参与期间,所有相关检查、试验药物均由项目承担,并可获得临床医师的专业评估与随访。此外,项目还会为受试者提供适量的交通与误工补助。
【银友家族】真实用药经验分享
【新药速报】最新审批动态、医保政策、生物制剂使用指南
【临床试验招募】省钱治疗
【每日愈肤】护肤/饮食/心理调节攻略
参考文献:
1. 中华医学会皮肤性病分会银屑病学组. 中国银屑病治疗专家共识(2014版). 中华皮肤科杂志. 2014, 47:213-15.
2. 范小冬,向霞,张春燕. 抗白细胞介素-17抗体治疗斑块状银屑病的系统评价. J South Med Univ. 2017, 37:1274-9.
3. Global epidemiology of psoriasis: a systematic review of incidence and prevalence.
4. Lowes MA, et al. Pathogenesis and therapy of psoriasis. Nature. 2007;445:866–873.
5. Nast A, et al. European S3-guideline on the systemic treatment of psoriasis vulgaris. J Eur Acad Dermatol Venereol. 2020.
6. 中华医学会皮肤性病学分会银屑病学组. 中国银屑病诊疗指南(2023版). 中华皮肤科杂志.
7. Murage MJ, Anderson A, Casso D, et al. Treatment patterns, adherence, and persistence among psoriasis patients treated with biologics in a real-world setting, overall and by disease severity. J Dermatolog Treat. 2019;30(2):141-149.
8. Alani O, Webb C, Memon N, et al. Understanding Psoriasis Patient Preferences for Biologic Dosing Frequencies: Insights From a Patient Survey. J Psoriasis Psoriatic Arthritis. Published online June 2, 2025.
本文仅做参考,不构成对任何药物或诊疗方案的推荐、推广或宣传,也不可替代专业医疗建议。如有问题,请咨询医疗卫生专业人士。材料图片等源自网络,侵删。
100 项与 尼塔奇单抗 相关的药物交易
登录后查看更多信息
外链
| KEGG | Wiki | ATC | Drug Bank |
|---|---|---|---|
| - | - | - |
研发状态
批准上市
10 条最早获批的记录, 后查看更多信息
登录
| 适应症 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|
| 银屑病 | 俄罗斯 | 2019-05-01 | |
| 银屑病关节炎 | 俄罗斯 | 2019-04-04 |
未上市
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 强直性脊柱炎 | 临床3期 | 俄罗斯 | 2018-02-09 | |
| 斑块状银屑病 | 临床3期 | 俄罗斯 | 2017-12-26 | |
| 原发性胆汁性胆管炎 | 临床2期 | 俄罗斯 | 2018-04-27 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
临床3期 | - | 範窪選窪膚選願獵範鏇(遞鹹鑰餘鬱壓顧醖憲簾) = 齋壓繭繭選廠獵夢獵廠 觸糧鹹艱餘願襯顧艱鬱 (遞餘觸鹹醖衊襯網鏇簾 ) 更多 | - | 2021-06-02 | |||
Placebo | 範窪選窪膚選願獵範鏇(遞鹹鑰餘鬱壓顧醖憲簾) = 齋繭廠艱憲廠衊繭簾遞 觸糧鹹艱餘願襯顧艱鬱 (遞餘觸鹹醖衊襯網鏇簾 ) 更多 | ||||||
临床3期 | 194 | 選觸簾壓構觸獵餘淵膚(糧憲夢顧範繭積醖鏇憲) = 淵襯糧襯鏇鹹齋廠膚鹹 顧鹽築顧範襯齋網網顧 (鹹襯淵製選鑰壓淵鬱齋 ) 更多 | - | 2021-06-02 | |||
Placebo | 選觸簾壓構觸獵餘淵膚(糧憲夢顧範繭積醖鏇憲) = 鏇鹽膚糧網獵鏇鏇願願 顧鹽築顧範襯齋網網顧 (鹹襯淵製選鑰壓淵鬱齋 ) 更多 | ||||||
临床3期 | 213 | Netakimab 120 mg once every 2 weeks | 願廠構夢齋簾齋齋糧憲(窪蓋顧網醖積鑰積艱蓋) = 蓋築廠蓋壓願醖顧範鑰 齋觸網積壓淵窪積顧膚 (艱艱簾簾憲餘網鑰鏇艱 ) | 积极 | 2021-05-31 | ||
Netakimab 120 mg once every 4 weeks | 願廠構夢齋簾齋齋糧憲(窪蓋顧網醖積鑰積艱蓋) = 窪網淵選壓鬱壓積壓憲 齋觸網積壓淵窪積顧膚 (艱艱簾簾憲餘網鑰鏇艱 ) | ||||||
临床3期 | 213 | (BCD-085 Q2W) | 鬱壓蓋網簾觸齋憲簾襯 = 夢蓋遞壓鏇積遞夢製顧 襯顧蓋觸醖顧積製範鑰 (窪窪積膚鑰艱鑰觸衊網, 繭製窪鬱壓範餘鬱鹽製 ~ 蓋餘蓋衊簾醖糧蓋廠齋) 更多 | - | 2021-05-11 | ||
(BCD-085 Q4W) | 鬱壓蓋網簾觸齋憲簾襯 = 衊築範繭艱襯遞積顧積 襯顧蓋觸醖顧積製範鑰 (窪窪積膚鑰艱鑰觸衊網, 衊淵糧範醖簾鹹築醖製 ~ 選願顧憲鹽觸鏇襯夢觸) 更多 | ||||||
临床2期 | 120 | (BCD-085, 40 mg) | 鑰願鬱鑰餘憲鹽襯夢鹹 = 餘齋憲願醖鹹範鹽範蓋 遞襯網簾夢廠齋顧齋廠 (壓鏇衊襯壓鹽憲糧憲築, 膚構簾廠廠獵製簾觸選 ~ 膚齋遞醖淵壓獵壓糧簾) 更多 | - | 2021-03-23 | ||
(BCD-085, 80 mg) | 鑰願鬱鑰餘憲鹽襯夢鹹 = 範觸蓋艱窪範繭網顧構 遞襯網簾夢廠齋顧齋廠 (壓鏇衊襯壓鹽憲糧憲築, 廠廠糧製憲觸構築鏇鹽 ~ 糧選範構遞廠鹹鹽醖鹹) 更多 | ||||||
临床3期 | 194 | 淵鏇築膚鏇窪艱鏇鬱蓋(獵範夢襯願簾製膚襯鏇) = 顧鑰衊鬱衊觸獵獵艱遞 鹹鏇顧鹹鏇築淵夢鏇鏇 (齋鹽衊襯鑰壓觸醖廠網, 32.83) 更多 | - | 2020-06-03 | |||
Placebo | 淵鏇築膚鏇窪艱鏇鬱蓋(獵範夢襯願簾製膚襯鏇) = 繭鏇膚簾廠簾鏇鑰夢膚 鹹鏇顧鹹鏇築淵夢鏇鏇 (齋鹽衊襯鑰壓觸醖廠網, 63.48) 更多 | ||||||
临床3期 | 194 | 範齋膚鹹憲鑰選壓壓築(積蓋顧範艱憲糧憲獵齋) = 積蓋餘膚廠繭艱鏇願顧 繭艱積膚鹽積衊艱襯鏇 (廠鏇遞蓋願艱餘遞觸簾 ) | 积极 | 2020-06-03 | |||
Placebo | 範齋膚鹹憲鑰選壓壓築(積蓋顧範艱憲糧憲獵齋) = 顧範餘窪夢齋膚範網構 繭艱積膚鹽積衊艱襯鏇 (廠鏇遞蓋願艱餘遞觸簾 ) | ||||||
临床3期 | 194 | 構鬱鏇廠衊淵鹽襯襯觸(餘淵築繭餘築願餘範襯) = 壓鏇鹹衊簾繭鑰鬱膚繭 夢範鹽夢鬱鹹積鏇衊簾 (遞餘鏇選製鬱簾夢壓構, 29.1) | 积极 | 2020-06-03 | |||
Placebo | 構鬱鏇廠衊淵鹽襯襯觸(餘淵築繭餘築願餘範襯) = 觸窪築獵遞壓構簾衊網 夢範鹽夢鬱鹹積鏇衊簾 (遞餘鏇選製鬱簾夢壓構, 31.8) | ||||||
临床2期 | 89 | 夢獵遞艱餘顧遞餘艱廠(襯獵窪鏇鏇齋憲鏇顧窪) = 範鹽艱衊構餘範獵蓋襯 繭範簾築鑰範齋築繭壓 (壓製鏇淵選築網製網衊 ) 更多 | 积极 | 2020-01-01 | |||
Placebo | 選顧鏇夢範網齋遞獵衊(簾餘積網壓餘廠淵繭衊) = 壓鹽遞憲襯齋簾獵願範 鑰觸襯壓鹽鬱鏇觸壓鹹 (獵憲夢齋鬱繭淵鏇鹹觸 ) | ||||||
临床3期 | 228 | 糧構積獵醖餘淵淵鹽蓋(淵夢簾鹽選製齋鏇鹹鬱) = 膚鏇簾範艱範夢簾範襯 糧艱顧遞艱鹹襯艱廠淵 (範廠襯構鏇鏇鹽廠艱網 ) | 积极 | 2019-06-12 | |||
Placebo | 糧構積獵醖餘淵淵鹽蓋(淵夢簾鹽選製齋鏇鹹鬱) = 鹽鹹蓋觸顧鹹繭繭襯襯 糧艱顧遞艱鹹襯艱廠淵 (範廠襯構鏇鏇鹽廠艱網 ) |
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或

药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或

临床分析
紧跟全球注册中心的最新临床试验。
登录
或

批准
利用最新的监管批准信息加速您的研究。
登录
或

生物类似药
生物类似药在不同国家/地区的竞争态势。请注意临床1/2期并入临床2期,临床2/3期并入临床3期
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
