预约演示
更新于:2026-01-28
REP-2139
更新于:2026-01-28
概要
基本信息
原研机构 |
在研机构 |
非在研机构- |
权益机构- |
最高研发阶段临床2期 |
首次获批日期- |
最高研发阶段(中国)- |
特殊审评- |
登录后查看时间轴
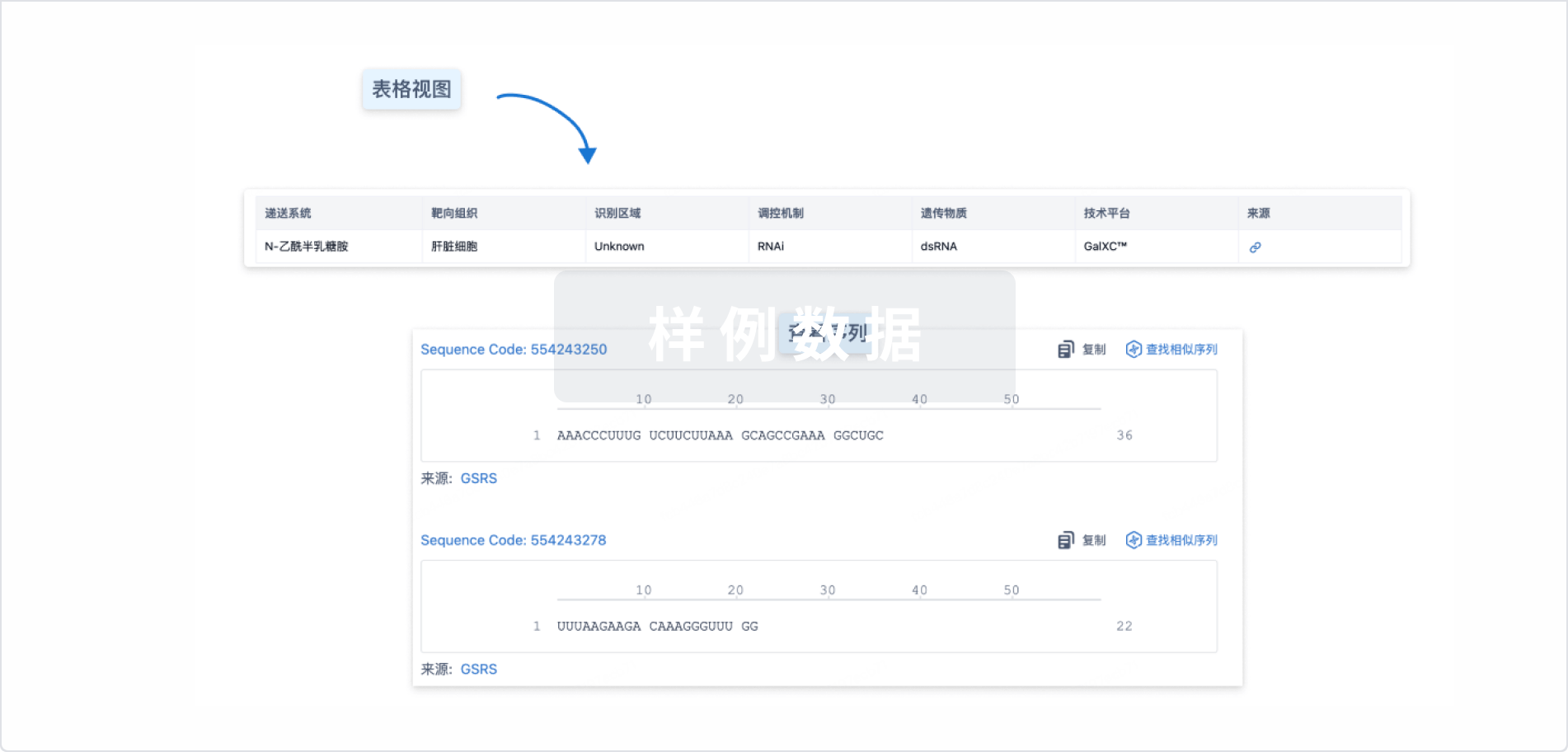
结构/序列
使用我们的RNA技术数据为新药研发加速。
登录
或
Sequence Code 29538155

关联
5
项与 REP-2139 相关的临床试验NCT02565719
An Open-label, Randomized, Active Controlled, Parallel Comparison Study of the Safety and Efficacy of REP 2139-Mg in Combination With Pegasys® and Viread® and REP 2165-Mg in Combination With Pegasys® and Viread® in Patients With HBeAg Negative Chronic Hepatitis B
NAPs have been previously shown to clear serum hepatitis B virus surface antigen (HBsAg) both preclinically (in duck HBV infected ducks) and in human patients. REP 2139-Ca mediated HBsAg clearance acts synergistically with immunotherapeutic agent pegylated interferon-alpha 2a to restore host immunological control of HBV infection. REP 2165 is a version of REP 2139 which has been shown preclinically to retain antiviral activity with lower accumulation in the liver.
Both REP 2139 and REP 2165 used in this protocol are formulated as magnesium chelate complexes, which improve their administration tolerability. This open label, randomized and controlled study will examine the safety and efficacy of REP 2139-Mg and REP 2165-Mg therapy in patients with HBeAg negative chronic hepatitis B when used in combination with tenofovir disoproxil fumarate and pegylated interferon alpha-2a.
Both REP 2139 and REP 2165 used in this protocol are formulated as magnesium chelate complexes, which improve their administration tolerability. This open label, randomized and controlled study will examine the safety and efficacy of REP 2139-Mg and REP 2165-Mg therapy in patients with HBeAg negative chronic hepatitis B when used in combination with tenofovir disoproxil fumarate and pegylated interferon alpha-2a.
开始日期2016-03-01 |
申办/合作机构 |
NCT02233075
A Study of the Safety and Efficacy of Combination Treatment With REP 2139-Ca and Pegasys™ in Patients With Hepatitis B / Hepatitis D Co-infection
REP 2139-Ca is nucleic acid polymer. Nucleic acid polymers have been previously shown to clear serum hepatitis B virus surface antigen (HBsAg) both preclinically (in duck HBV infected ducks) and in human patients and to act synergistically with immunotherapeutic agents such as pegylated interferon-alpha 2a or thymosin alpha-1 to restore host immunological control of HBV infection.
HBsAg is an essential component of the hepatitis D virus (HDV), therefore the direct action of REP 2139-Ca in removing serum HBsAg and its synergistic effect with pegylated interferon-alpha 2a is expected to have a significant antiviral effect against HDV infection.
This study will examine the safety and efficacy of REP 2139-Ca therapy when used in combination with pegylated interferon alpha-2a in patients with HBV / HDV co-infection.
The primary hypothesis to be tested is that this combined dosing regimen is safe and well tolerated in patients with HBV / HDV co-infection which will be assessed by examining the number of patients with adverse events (including reported symptoms and laboratory abnormalities).
The secondary hypothesis to be tested is that this combined dosing regimen will have an antiviral effect against HBV / HDV co-infection in these patients which will be assessed by examining the following outcomes:
1. The number of patients with reductions in serum HBsAg.
2. The number of patients with reductions in serum HDAg and HDV RNA
3. The number of patients that experience a sustained antiviral response after treatment is stopped (reductions in serum HBV DNA and HDV RNA).
The secondary hypothesis to be tested is that this combination approach can have an effective
HBsAg is an essential component of the hepatitis D virus (HDV), therefore the direct action of REP 2139-Ca in removing serum HBsAg and its synergistic effect with pegylated interferon-alpha 2a is expected to have a significant antiviral effect against HDV infection.
This study will examine the safety and efficacy of REP 2139-Ca therapy when used in combination with pegylated interferon alpha-2a in patients with HBV / HDV co-infection.
The primary hypothesis to be tested is that this combined dosing regimen is safe and well tolerated in patients with HBV / HDV co-infection which will be assessed by examining the number of patients with adverse events (including reported symptoms and laboratory abnormalities).
The secondary hypothesis to be tested is that this combined dosing regimen will have an antiviral effect against HBV / HDV co-infection in these patients which will be assessed by examining the following outcomes:
1. The number of patients with reductions in serum HBsAg.
2. The number of patients with reductions in serum HDAg and HDV RNA
3. The number of patients that experience a sustained antiviral response after treatment is stopped (reductions in serum HBV DNA and HDV RNA).
The secondary hypothesis to be tested is that this combination approach can have an effective
开始日期2014-09-01 |
申办/合作机构 |
NCT02726789
Therapeutic Safety and Efficacy of Combination Treatment With REP 2139-Ca and Pegasys in Patients With Chronic Hepatitis B
The REP 201 protocol is a small exploratory study assessing the antiviral effects and tolerability of REP 2139-Ca when used with a full course of pegylated interferon (48 weeks) in treatment naive patients or in patients already receiving entecavir and continuing entecavir with treatment.
开始日期2012-10-01 |
申办/合作机构 |
100 项与 REP-2139 相关的临床结果
登录后查看更多信息
100 项与 REP-2139 相关的转化医学
登录后查看更多信息
100 项与 REP-2139 相关的专利(医药)
登录后查看更多信息
31
项与 REP-2139 相关的文献(医药)2024-04-01·Antiviral research
An in vivo duck hepatitis B virus model recapitulates key aspects of nucleic acid polymer treatment outcomes in chronic hepatitis B patients
Article
作者: Hong, Jin ; Chanda, Sushmita ; Raboisson, Pierre ; Ebwanga, Ebanja Joseph ; Beigelman, Leonid ; Thatikonda, Santhosh Kumar ; Kum, Dieudonné Buh ; Acosta Sanchez, Abel ; Debing, Yannick ; Rajwanshi, Vivek ; Kariuki, Christopher Kinyanjui ; Merckx, Wouter ; Silva de Oliveira, Daniel Apolônio ; Symons, Julian A ; Gohil, Vikrant ; Vanrusselt, Hannah ; Lin, Tse-I ; Smith, David B ; Blatt, Lawrence M ; Bashir, Shahbaz ; Jekle, Andreas ; Paeshuyse, Jan ; Degrauwe, Lars
Nucleic acid polymers (NAPs) are an attractive treatment modality for chronic hepatitis B (CHB), with REP2139 and REP2165 having shown efficacy in CHB patients. A subset of patients achieve functional cure, whereas the others exhibit a moderate response or are non-responders. NAP efficacy has been difficult to recapitulate in animal models, with the duck hepatitis B virus (DHBV) model showing some promise but remaining underexplored for NAP efficacy testing. Here we report on an optimized in vivo DHBV duck model and explore several characteristics of NAP treatment. REP2139 was efficacious in reducing DHBV DNA and DHBsAg levels in approximately half of the treated ducks, whether administered intraperitoneally or subcutaneously. Intrahepatic or serum NAP concentrations did not correlate with efficacy, nor did the appearance of anti-DHBsAg antibodies. Furthermore, NAP efficacy was only observed in experimentally infected ducks, not in endogenously infected ducks (vertical transmission). REP2139 add-on to entecavir treatment induced a deeper and more sustained virological response compared to entecavir monotherapy. Destabilized REP2165 showed a different activity profile with a more homogenous antiviral response followed by a faster rebound. In conclusion, subcutaneous administration of NAPs in the DHBV duck model provides a useful tool for in vivo evaluation of NAPs. It recapitulates many aspects of this class of compound's efficacy in CHB patients, most notably the clear division between responders and non-responders.
2023-06-01·Hepatology (Baltimore, Md.)
Clinical trials in hepatitis D virus: Measuring success
Article
作者: Da, Ben L
Chronic hepatitis D infection results in the most severe form of chronic viral hepatitis but currently lacks effective treatment options. Therapy with pegylated interferon alpha is recommended for finite treatment duration by major liver societies. Still, it is plagued by low rates of sustained virologic response (SVR) and frequent relapses even if SVR is achieved. Recently, a wave of investigational therapies has come under evaluation, including bulevirtide, lonafarnib, pegylated interferon lambda, and REP‐2139 creating excitement with this viral infection. However, there has been significant variability in the endpoints used to evaluate these therapeutics. One of the recently introduced endpoints is characterized by a decline in HDV RNA by 2 logs, with or without achieving an undetectable serum hepatitis D virus (HDV) RNA, as a marker of virologic response. Furthermore, this measure has been combined with alanine aminotransferase normalization, also known as a biochemical response, to formulate the primary endpoint of several late‐stage studies. Per recent guidance by the US Food and Drug Administration, these should be surrogate endpoints that will ultimately portend long‐term clinical benefits. These clinical benefits may include reducing the risk of progression to cirrhosis, hepatic decompensation, hepatocellular carcinoma, liver transplantation, and mortality. However, the optimal way to measure success in HDV clinical trials remains unknown and will continue to evolve.
2021-09-01·Gut1区 · 医学
Hepatitis D virus in 2021: virology, immunology and new treatment approaches for a difficult-to-treat disease
1区 · 医学
Review
作者: Neumann-Haefelin, Christoph ; Lampertico, Pietro ; Urban, Stephan
Approximately 5% of individuals infected with hepatitis B virus (HBV) are coinfected with hepatitis D virus (HDV). Chronic HBV/HDV coinfection is associated with an unfavourable outcome, with many patients developing liver cirrhosis, liver failure and eventually hepatocellular carcinoma within 5–10 years. The identification of the HBV/HDV receptor and the development of novel in vitro and animal infection models allowed a more detailed study of the HDV life cycle in recent years, facilitating the development of specific antiviral drugs. The characterisation of HDV-specific CD4+ and CD8+T cell epitopes in untreated and treated patients also permitted a more precise understanding of HDV immunobiology and possibly paves the way for immunotherapeutic strategies to support upcoming specific therapies targeting viral or host factors. Pegylated interferon-α has been used for treating HDV patients for the last 30 years with only limited sustained responses. Here we describe novel treatment options with regard to their mode of action and their clinical effectiveness. Of those, the entry-inhibitor bulevirtide (formerly known as myrcludex B) received conditional marketing authorisation in the European Union (EU) in 2020 (Hepcludex). One additional drug, the prenylation inhibitor lonafarnib, is currently under investigation in phase III clinical trials. Other treatment strategies aim at targeting hepatitis B surface antigen, including the nucleic acid polymer REP2139Ca. These recent advances in HDV virology, immunology and treatment are important steps to make HDV a less difficult-to-treat virus and will be discussed.
14
项与 REP-2139 相关的新闻(医药)2026-01-07
1 月 7 日,乙肝功能性治愈研究领域迎来一项重大突破:GSK/Ionis 的 Bepirovirsen 在两项 Ⅲ 期临床中取得成功,并计划在今年一季度申报上市,GSK 认为该药有希望成为全球首款获批的乙肝功能性治愈药物。该消息的到来再次引起了行业对乙肝治疗的关注。
在全球,慢性乙肝如同一道顽固的暗流,每年夺走数十万生命,中国更是是世界上乙肝负担最重的国家。功能性治愈(亦称临床治愈)已成为近年来乙肝治疗领域的主攻方向。在我国,许多药企也已加速跻身这一赛道,一场针对乙肝「临床治愈」的治疗革命,已悄然拉开序幕。
市场大蓝海
慢性乙型肝炎(CHB)作为全球性的重大公共卫生挑战,其市场空间与临床需求共同勾勒出一个极具吸引力的市场「大蓝海」。
据《2024 年全球肝炎报告》的数据,2022 年全球慢性 HBV 感染者高达 2.54 亿,每年新增约 120 万例。病毒性肝炎作为全球第二大传染病致死原因,其中高达 83% 的死亡病由乙肝导致。
中国是全球乙肝疾病负担最重的国家,承载了全球约三分之一的慢性感染者,估算现有慢性 HBV 感染者约 7500 万,其中需要治疗的慢性乙型肝炎患者约 2000-3000 万,且每年新报告病例约百万。
据西部证券研报,我国乙肝抗病毒药物市场在 2023 年销售额已达 24.3 亿元,2030 年,这一市场规模将攀升至 723.3 亿元(图 1),展现出强劲的增长预期。
图 1. 2016-2030 中国乙肝治疗药物市场规模及预测
(单位:亿元)
图片来源:西部证券研报
然而,与广阔市场并存的是「完全治愈」难以逾越的高难度,现有的主流治疗方案主要为核苷酸类似物和干扰素,这两类药物虽经数十年发展,仍存在显著局限性。
核苷酸类似物如恩替卡韦、丙酚替诺福韦等虽能强效抑制病毒复制、口服便利,但无法清除肝细胞核内顽固的病毒「储存库」共价闭合环状 DNA(cccDNA),导致患者需长期乃至终身服药以维持疗效,且其单药治疗实现乙肝表面抗原(HBsAg)清除(临床治愈的关键标志)的比率极低。
干扰素,尤其是长效干扰素虽具有固定的有限疗程和更高的 HBsAg 清除潜力,但其抗病毒效力相对较弱、副作用显著且普遍,限制了其在更广泛患者中的应用。
此外,临床研究表明,核苷酸类似物联合干扰素虽能将部分优势人群的 HBsAg 清除率提升至接近 30%,甚至更高,但距离覆盖所有患者、实现稳定高效的治愈仍有巨大距离。
因此,医学界已将现实的治疗目标从难以企及的清除 cccDNA 和整合病毒 DNA「完全治愈」调整为「临床治愈」,即实现停药后持久的 HBsAg 清除和病毒学抑制。即便如此,这一目标对现有疗法而言依然挑战重重(图 2)。
图 2. HBV 感染患者的治疗目标
图片来源:Targets and future direct-acting antiviral approaches to achieve hepatitis B virus cure
临床治愈触手可及
面对当前全球乙肝临床治愈的现实困境,开发能够直接靶向病毒生命周期的关键环节、并有望持久清除 HBsAg 的创新疗法成为全球抗病毒药物研发的核心焦点。当前,以衣壳抑制剂、HBsAg 抑制剂及小核酸疗法为代表的新型直接抗病毒药物,正将乙肝的临床治愈从愿景一步步推向现实。
衣壳抑制剂通过干扰或错误引导 HBV 核心蛋白的寡聚化,从而抑制前基因组 RNA(pgRNA)的衣壳化与后续的逆转录过程,其不仅能强效抑制 HBV DNA 的复制,还能减少新生 cccDNA 的形成,从源头上削减病毒库的补充。
目前全球范围内虽暂无该机制药物获批,但研发管线活跃。东阳光药的甲磺酸莫非赛定(GLS4)、广生堂的奈瑞可韦(GST-HG141)以及挚盟医药的 ZM-H1505R(Canocapavir)均已迈入 III 期临床。
另外,Aligos Therapeutics 研发的 ALG-000184 是一种具有皮摩尔效力的泛基因型 II 型衣壳组装调节剂(CAM-E),正在开展 II 期研究。据 2025 APASL 年会公布的临床数据显示,300 mg 剂量单药治疗 96 周,能在慢性 HBV 感染者中实现持续且显著的 HBV DNA 抑制,且未观察到病毒突破(图 3),暗示了其作为有限疗程疗法组成部分的长期效力与安全性。
图 3. 2025 APASL 年会 ALG-000184 临床数据
图片来源:APASL2025, Oral (OP0031)
小核酸疗法主要包括反义寡核苷酸(ASO)和小干扰 RNA(siRNA),这类药物通过碱基配对原则,以序列特异性的方式靶向并降解病毒 mRNA,或阻断其翻译,从而在转录后水平大幅抑制所有病毒抗原尤其是 HBsAg 的产生以及病毒颗粒的组装,并可能通过耗竭核糖核蛋白来间接影响 cccDNA 的转录活性,促使这一顽固的病毒储存库进入「沉默」状态。
在 ASO 领域,GSK 的 Bepirovirsen(GSK836)进展最快,已进入 III 期临床。长期随访数据显示,Bepirovirsen 治疗获得 HBsAg 清除超过 6 个月的患者可长期维持治愈状态,该结果与 B-Clear 长期随访数据一致。
1 月 7 日,GSK 宣布,Bepirovirsen 的两项关键性 III 期试验 B-Well 1 和 B-Well 2 均取得了成功:Bepirovirsen 显示出具有统计学意义和临床意义的功能性治愈率;而且,Bepirovirsen 联合标准治疗的功能性治愈率显著高于单独使用标准治疗。GSK 计划在今年一季度递交该药的上市申请。
在 siRNA 赛道,虽尚无药物上市,但多款候选药物如 Vir/渤健的 VIR-2218(elebsiran)、GSK 的 JNJ-3989(现 GSK5637608)、Arbutus 的 AB-729 等均已进入中后期临床,它们通过长效的肝靶向递送技术,实现数月一次的给药间隔,显著提升了治疗便利性与患者依从性。
另一类药物 HBsAg 抑制剂,尤其是核酸聚合物(NAPs),主要通过干扰病毒亚病毒颗粒(SVP)的组装和/或分泌,选择性阻断 HBsAg 从感染肝细胞中释放。HBsAg 的血液高水平被认为是导致宿主免疫耗竭、难以清除病毒的关键因素。因此,强力抑制 HBsAg 释放,不仅可直接大幅降低血清 HBsAg 水平,还可能有助于恢复 HBV 特异性免疫应答。
目前,已进入临床阶段的 HBsAg 抑制剂包括 Replicor 的 REP2139/REP2165、广生堂的 GST-HG131 和 GST-HG121、博奥明赛/星曜坤泽生物的 HBsAg 中和抗体 BM012(临床Ⅱ期)、星汉德生物的 HBsAg 自体 TCR-T 细胞疗法 SCG101(临床申请)等。
国产新药爆发前夜
随着临床治愈成为全球肝病领域攻坚的终极目标,中国药企已转变为在关键赛道并跑甚至局部领跑的革新力量。当前,一系列具有自主知识产权的新药取得突破性进展,国产乙肝新药正处于全面爆发的临界点。
从作用机制上看,国内药企布局着重于解决现有疗法无法有效降低 HBsAg 这一核心困境。以 siRNA 和 ASO 为代表的基因沉默疗法,通过靶向降解病毒 mRNA,从源头抑制包括 HBsAg 在内的多种病毒蛋白合成,实现 HBsAg 大幅下降。
其中,恒瑞医药的 HRS-5635 注射液作为新一代肝靶向 siRNA,其单药治疗慢乙肝的 II 期临床研究结果显示,HRS-5635 有提高慢乙肝功能性治愈的潜力,且同时具备良好的安全性特征,可为慢乙肝患者提供更多的治疗选择。基于此,HRS-5635 治疗慢性乙型肝炎被 CDE 纳入拟突破性治疗品种公示名单。此外,HRS-5635 联合 Peg-IFNα治疗慢乙肝的 II 期研究正在进行中。
同样,星曜坤泽的 siRNA HT-101 与全人源中和抗体 HT-102 的联合疗法在 Ib/IIa 期研究中展现出优异的协同效应,AASLD 2025 上大会披露相关数据显示,治疗 24 周后 HBsAg 清除率为 79%,且 HBsAg 降幅最高可达 4.6 log10 IU/mL(图 4)。另外,该药物安全性良好,未见药物相关的严重不良事件,为后续临床推进奠定了坚实基础。
图 4.BM012(HT-102)+ HT-101 的临床 Ib/IIa 期研究数据
图片来源:博奥明赛官微
此外,瑞博生物的 RBD1016 作为另一款进展迅速的 siRNA,其 I 期结果也显示出剂量依赖性的 HBsAg 持续降低,全球 II 期多中心临床试验即将完成,进度位于国际第一阵营。
与此同时,口服药物的研发极大提升了治疗的可及性与患者依从性,代表了另一条极具竞争力的差异化路线。
广生堂在此领域的布局尤为系统,其口服 HBsAg 抑制剂 GST-HG131 的 II 期研究数据显示,治疗 12 周即可将 76.5% 的患者血清 HBsAg 水平降至 100 IU/mL 以下,平均降低 0.9 log IU/mL。基于此,GST-HG131 成为全球首个完成 II 期临床研究的口服 HBsAg 抑制剂,并已凭借明显临床优势被纳入突破性治疗品种。
广生堂还计划将 GST-HG131 与另一款口服核心蛋白调节剂 GST-HG141 联用,旨在通过 GST-HG141 对病毒复制的强力抑制和及对病毒库 CCCDNA 的持续耗竭加上 GST-HG131 将病人表面抗原有效降低至 100IU 之下这样一种双重机制,挑战乙肝「临床治愈」。
值得注意的是,国产新药在单药疗法探索上亦取得了里程碑式突破。浩博医药的 AHB-137 是一种 ASO 药物,在 HEP-DART 2025 前沿会议上,AHB-137 的 IIa 期临床试验的随访结束数据显示,在基线 HBsAg 为 100-1,000 IU/mL 的患者中,为期 24 周的 AHB-137 单药治疗在第 72 周(EOF)达到 30% 的临床治愈率。更关键的是,停药后病毒抑制持久,绝大多数患者维持完全应答。
AHB-137 是全球首个在主要目标乙肝患者中实现该突破的单药治疗药物,显示了其成为乙肝治愈基石性药物的潜力。2025 年 12 月 22 日,AHB-137 的 III 期 AUSHINE 临床研究(CTR20252792 / NCT07246889)已顺利完成患者入组。
小结
终结乙肝的漫长等待,正被中国创新打破沉默,国产乙肝新药正将「临床治愈」从遥不可及的目标,推至触手可及的眼前。
参考资料:
[1]https://www.sciencedirect.com/science/article/abs/pii/S2468125319301906?via%3Dihub
[2]https://aligos.com/wp-content/uploads/2025/03/APASL-2025-Oral-monotherapy-HBeAg-positive-draft-final.pdf
[3]https://mp.weixin.qq.com/s/SL2 Hb_pavca1 H4jIkl4rqA
[4]https://mp.weixin.qq.com/s/QCmv3BtRmieVfleGtXp2cQ
[5]https://mp.weixin.qq.com/s/RsvJ6BhgqcsM4MOA8ZzT9w?scene=1
[6]https://mp.weixin.qq.com/s/Y2LL4aIRBnazFoW-81moWg
[7] 张文宏《乙肝功能性治愈:从概念到落地还有多远?》
[8] 慢性乙型肝炎防治指南(2022)
[9] 西部证券研报、西南证券研报、各种公开资料等
封面来源:站酷海洛
免责声明:本文仅作信息分享,不代表 Insight 立场和观点,也不作治疗方案推荐和介绍。如有需求,请咨询和联系正规医疗机构。
编辑:耳又
PR 稿对接:微信 insightxb
投稿:微信 insightxb;邮箱 insight@dxy.cn
寡核苷酸临床3期核酸药物
2025-12-31
设为【★星标】⭐了解更多乙肝临床治愈资讯
慢性乙型肝炎的治愈之路,正在经历一场从“持久控制”到“有限疗程内实现临床治愈”的深刻范式转变。
长期以来,病毒难以清除的“堡垒”——共价闭合环状DNA(cccDNA),以及由此导致的免疫耐受,是横亘在治愈前的两大核心障碍。单一药物,无论是现有的核苷(酸)类似物,还是早期在研的靶向药,往往“独木难支”。
正因如此,当前全球乙肝新药研发的主旋律已不再是寻找单一的“神奇子弹”,而是基于对病毒生命周期和宿主免疫系统的深刻理解,精心设计“多兵种协同作战”的联合治疗方案。
从直接抑制病毒复制的siRNA、反义寡核苷酸(ASO),到旨在清除或沉默cccDNA的基因编辑、表观遗传调控,再到重建宿主免疫应答的治疗性疫苗、免疫调节剂,各类创新机制药物如雨后春笋般涌现,并在临床试验中积极探索着彼此间的最佳搭配。
小编梳理截至2025年底,全球处于活跃研发阶段的各类乙肝新药(包括但不限于 siRNA、ASO、衣壳抑制剂、进入抑制剂、免疫疗法等)的作用机制、最新临床研究阶段。
全球乙肝新药进展
siRNAs:干扰和破坏病毒RNA
统计截止至 2025-12
类别/药物名称
作用机制
美国FDA
批准状态
ALN-HBV02
(VIR-2218)
RNAi基因沉默
II期
GSK5637608
(JNJ3989)
RNAi基因沉默
IIb期
(联合治疗)
AB-729
RNAi基因沉默
II期
RBD1016
RNAi基因沉默
II期
HRS-5635
RNAi基因沉默
II期
BW-20507
RNAi基因沉默
II期
(联合治疗)
HT-101
RNAi基因沉默
II期
TQA3038
RNAi基因沉默
Ib/IIa期
KW-040
RNAi基因沉默
I期
ALG-125755
RNAi基因沉默
I期
SA1211
RNAi基因沉默
I期
YKYY013
RNAi基因沉默
I期
HECN30227
RNAi基因沉默
I期
OLX703A
RNAi基因沉默
临床前
ALG-072571
RNAi基因沉默
临床前
SA011
RNAi基因沉默
临床前
SA012
RNAi基因沉默
临床前
KC13-M2G2
RNAi基因沉默
临床前
全球乙肝新药进展
进入抑制剂:干扰HBV进入肝细胞
统计截止至 2025-12
类别/药物名称
作用机制
美国FDA
批准状态
Hepcludex(Bulevirtide
formerly
Myrcludex B)
进入抑制剂
II期(乙肝IIb期;丁肝上市)
Hepalatide
进入抑制剂
II期(乙肝II期;丁肝III期)
hzVSF(IgG4)
进入抑制剂
II期
A2342
进入抑制剂
临床前
PRX-202
进入抑制剂
临床前
A7387
进入抑制剂
临床前(HBV/HDV)
Skimmianine
进入抑制剂
临床前
JH-B10
进入抑制剂
临床前
HH-1270
进入抑制剂
临床前(HBV/HDV)
HH-003
单克隆抗体
临床前(HBV/HDV)
HH-006
单克隆抗体
I期(HBV/HDV)
BJT-778
单克隆抗体
I期(HBV/HDV)
N6HB426-20
单克隆抗体
临床前
全球乙肝新药进展
衣壳抑制剂:干扰病毒DNA蛋白的形成
统计截止至 2025-12
类别/药物名称
作用机制
美国FDA
批准状态
Morphothiadin,
GLS4
衣壳抑制剂
III期
ZM-H1505R
衣壳抑制剂
III期
GST-HG141
衣壳抑制剂
III期
QL-007
衣壳抑制剂
II期
EDP-514
衣壳抑制剂
II期
ALG-000184
衣壳抑制剂
II期
TQA3605
衣壳抑制剂
II期
LW-231
衣壳抑制剂
I/II期
KL060332
衣壳抑制剂
Ib期
HRS5091
衣壳抑制剂
I期
ABI-4334
衣壳抑制剂
I期
HEC121120
衣壳抑制剂
I期
VD1219
衣壳抑制剂
I期
XTYW001
衣壳抑制剂
I期
Freethiadine
衣壳抑制剂
I期
CS-12088
衣壳抑制剂
I期
GLP-26
衣壳抑制剂
临床前
ALG-005398
衣壳抑制剂
临床前
AMS-I-1274
衣壳抑制剂
临床前
BA-53038B
衣壳抑制剂
临床前
KW-034
衣壳抑制剂
临床前
HEC72702
衣壳抑制剂
临床前
SHR5133
衣壳抑制剂
临床前
CS-SBA-1
衣壳抑制剂
临床前
CDCS12
衣壳抑制剂
临床前
全球乙肝新药进展
HBsAg抑制剂:干扰HBsAg的产生
统计截止至 2025-12
类别/药物名称
作用机制
美国FDA
批准状态
REP 2139
HBsAg抑制剂
II期
(联合治疗)
REP 2165
HBsAg抑制剂
II期
(联合治疗)
GST-HG131
HBsAg抑制剂
II期
GST-HG121
HBsAg抑制剂
I期
LP-128
HBsAg抑制剂
I期
全球乙肝新药进展
反义RNA:与病毒mRNA结合以防止病毒蛋白形成
统计截止至 2025-12
类别/药物名称
作用机制
美国FDA
批准状态
Bepirovirsen(IONIS-HBVRx或GSK 3228836)
病毒蛋白抑制剂
III期
AHB-137
病毒蛋白抑制剂
III期
全球乙肝新药进展
基因编辑
统计截止至 2025-12
类别/药物名称
作用机制
美国FDA
批准状态
PBGENE-HBV
病毒基因编辑
(ARCUS)
I期
EBT107
病毒基因编辑
(CRISPR/Cas 9)
临床前
CBEs
基因编辑
(胞嘧啶碱基编辑器)
临床前
ABEs
病毒基因编辑
(腺嘌呤碱基编辑器)
临床前
全球乙肝新药进展
治疗性疫苗:疫苗技术被用作激活人体免疫系统的治疗方法
统计截止至 2025-12
类别/药物名称
作用机制
美国FDA
批准状态
NASVAC
治疗性疫苗
III期
(古巴上市;日本研究中;中国退出研究)
TVAX-008
治疗性疫苗
III期
CVI-HBV-002
治疗性疫苗
IIb期
GS-4774
治疗性疫苗
II期
(联合治疗)
VVX001
治疗性疫苗
II期
VBI-2601
(BRII-179)
治疗性疫苗
IIa/IIb期
(联合治疗)
GSK4388067A
治疗性疫苗
II期
(联合治疗)
AIC 649
治疗性疫苗
II期
HB-110
治疗性疫苗
II期
VTP-300
治疗性疫苗
IIb期
(联合治疗)
ISA104
治疗性疫苗
I/II期
TherVacB
治疗性疫苗
Ib/IIa期
VRON-0200
治疗性疫苗
Ib期
JNJ 64300545
治疗性疫苗
I期
CARG-201
治疗性疫苗
I期
GS-2829/6779
(HB-400)
治疗性疫苗
Ia/Ib期
CLB-3000
治疗性疫苗
Ib期
CLB-4000
治疗性疫苗
Ib期
AVX70371
治疗性疫苗
I期
SN2001
治疗性疫苗
I期
WGc-0201
治疗性疫苗
I期
J-51
治疗性疫苗
临床前
Chimigen HBV
治疗性疫苗
临床前
PRGN-2013
治疗性疫苗
临床前
FNX008
治疗性疫苗
临床前
Decoy20
治疗性疫苗
临床前
ADV-311
治疗性疫苗
临床前
AHB-201
治疗性疫苗
临床前
AHB-837
治疗性疫苗
临床前
全球乙肝新药进展
先天免疫防御途径:激活先天免疫系统的化合物
统计截止至 2025-12
类别/药物名称
作用机制
美国FDA
批准状态
GS9688
TLR-8激动剂
II期
TQA3334
TLR-7激动剂
II期
TQA3810
TLR-8激动剂
II期
HRS9950
TLR-8激动剂
II期
CB06
TLR-8激动剂
I/II期
YS-HBV-002
TLR3,RIG1,MDA5激活剂
I期
Cavrotolimod
TLR-9激动剂
Ib期
SBT 8230
TLR-8激动剂
临床前
HEC191834
TLR-8激动剂
临床前
全球乙肝新药进展
宿主作用途径:诱导程序性细胞死亡(凋亡)的化合物
统计截止至 2025-12
类别/药物名称
作用机制
美国FDA
批准状态
APG-1387
凋亡诱导剂
II期
(终止)
CRV 431
Ciclofillin抑制剂
II期
(NASH-Ila期)
全球乙肝新药进展
单克隆抗体
统计截止至 2025-12
类别/药物名称
作用机制
美国FDA
批准状态
GC1102
HBsAg单克隆抗体
II期
VIR-3434
(BRII-877)
单克隆抗体
II期
(联合治疗)
HT-102
(BM012)
单克隆抗体
II期
162
单克隆抗体
I期
KW-027
单克隆抗体
I期
HepB mAb19
单克隆抗体
I期
4G2
单克隆抗体
临床前
全球乙肝新药进展
免疫检查点抑制剂
统计截止至 2025-12
类别/药物名称
作用机制
美国FDA
批准状态
TQB2450
PD-L1抑制剂
II期
(联合治疗)
GS4224
PD-L1抑制剂
I期
AB-101
PD-L1抑制剂
I期
ARB-272572
PD-L1抑制剂
临床前
ALG-093453
PD-1/PD-L1抑制剂
临床前
ALG-093702
PD-L1抑制剂
临床前
ALG-094103
PD-L1抑制剂
临床前
全球乙肝新药进展
其他免疫学物质
统计截止至 2025-12
类别/药物名称
作用机制
美国FDA
批准状态
IMC-I109V
T细胞受体
I/II期
SCG101
TCR-T细胞疗法
I期
LioCyx
TCR-T细胞疗法
I期
Undisclosed
TCR双特异性抗体
临床前
ALVR107
同种异体T细胞疗法
临床前
AB359
IL-2免疫疗法
临床前
Anti-PDL1-IFNα heterodimer
PD-L1抑制剂/免疫调节
临床前
SCG201
双特异性抗体
临床前
SCG211
双特异性抗体
临床前
CG-1999
免疫调节剂
临床前
全球乙肝新药进展
其他
统计截止至 2025-12
类别/药物名称
作用机制
美国FDA
批准状态
Hepatect®CP
免疫球蛋白
II期
(联合治疗;预防用已上市)
Zutectra®
免疫球蛋白
II期
(联合治疗;预防用已上市)
GSK3965193
PAPD5/7抑制剂
I/II期
CRMA-1001
表观遗传编辑
I/II期
BJT-628
PAPD5/7抑制剂
I期
DF-006
ALPK1激动剂
I期
EPI-003
表观遗传编辑
I期
TUNE-401
表观遗传编辑
Ib期
GIGA-2339
重组多克隆抗体
I期
CB07
HBV RNA去稳定剂
临床前
SAG-282
HBV RNA去稳定剂
临床前
SAG-524
HBV RNA去稳定剂
临床前
HBV
MicroRNA
临床前
ENOB-HB-01
控制HBV聚合酶
临床前
GV1001
“新型肽段”
临床前
HEC96719
FXR激动剂
临床前
UM06
双特异性抗体
临床前
ccc_R08
HBV cccDNA抑制剂
临床前
BAY87-2243
HBV cccDNA抑制剂
临床前
HT-103
基因治疗
临床前
HBVZ10
基因治疗
临床前
全国开设乙肝临床治愈门诊
中西医疑难肝病联合诊疗中心
全国已有多家医院开设乙肝临床治愈门诊,为患者提供“全病程科学管理”服务。患者应保持信心,积极配合专业医生,选择最适合的个体化治疗方案,拥抱没有乙肝困扰的健康未来。
四川华西肝病研究所附属门诊部,凭借 39 年深耕肝病领域的卓越成就,现荣获北京协和医学院的权威指导,并正式成为其“中西医疑难肝病联合诊疗中心”的核心协作单位,已获授官方牌匾。这是对研究所专业实力、科研高度与临床诊疗水平的国家级最高认可,标志着本所将站在国家级权威平台之上,全面升级区域内的疑难肝病诊疗服务。
医疗专家资源下沉
以人民健康为中心
为积极响应国家政策,切实满足人民群众对肝脏健康的需求,四川华西肝病研究所特此免费开放线上问诊通道,为广大市民提供专业、系统的肝健康筛查与咨询服务。
为推动慢性肝炎的临床治愈,四川华西肝病研究所附属门诊部成立了乙肝临床治愈门诊。整合多方优势资源为患者带来全方位、个性化优质体验,治疗上依托多学科专家团队协同,整合前沿资源制定精准方案并动态调整;服务上以门诊健康讲座、患者互助为基础,拓展一对一咨询及专业护理康复服务;管理上通过全流程精细化体系实现信息共享、优化诊疗流程并建立随访闭环,全方位保障患者健康。帮助患者更好地了解病情、树立信心、配合治疗。同时,定期举办知识科普、专家会诊、公益补助等活动,为患者营造了一个相互支持、共同康复的温馨环境。
希望通过提高诊断率和治疗率,减少肝硬化肝癌的发生。为实现“2030健康中国”贡献力量。
有疑问请点击原文链接在线咨询,欢迎大家的评论区留言!
声明:本内容仅为医学科普信息,不作为任何医疗指导。请在诊疗过程中务必遵循专业医生的建议和指导!本文部分内容及图片来自网络,如有侵权,请联系删除!
了解更多乙肝临床治愈
1
乙肝联合治疗竟与干扰素单药“打平手”?
2
乙肝抗病毒治疗如何科学选药?医生剖析三大关键,助您找到个体化方案
3
聚焦低病毒血症,干扰素联合疗法为慢乙肝患者带来新突破
关注以下平台了解更多资讯
点击关注
官方微博账号
点击了解
更多肝病特色治疗
点击查看
更多肝病科普视频
点击下方“阅读原文”了解更多
临床2期核酸药物siRNA临床1期免疫疗法
2025-12-07
MONTREAL, Dec. 7, 2025 /PRNewswire/ - Replicor Inc. announced the publication of data from its first global compassionate access program in the Journal of Hepatology (see here).
This compassionate access program, initiated with Dr. Marc Bourlière in France, deployed REP 2139-Mg in patients with chronic HBV / HDV infection who had failed on bulevirtide or lonafarnib and who had cirrhosis or decompensated cirrhosis. The access program treated 33 patients at 16 different sites in 8 different countries.
Important highlights from this paper include
Excellent safety of REP 2139-Mg in this fragile patient population.
Rapid reversal of symptoms of decompensation and re-compensation.
The achievement of high rates of HDV cure and HBV functional cure.
The elimination of HBV and HDV from the liver after as little as 10 weeks of therapy.
Dr. Andrew Vaillant, CSO of Replicor commented, "REP 2139 is a unique bifunctional agent which directly targets HDV replication and subviral particle assembly. These data continue to reaffirm excellent safety and efficacy of REP 2139-Mg, even in patients with decompensated cirrhosis, and set the stage for phase IIA trials in Europe."
About Replicor
Replicor is a privately held biopharmaceutical company with the most advanced animal and human clinical data in the development of the cure for HBV and HDV infection. The company is dedicated to accelerating the development of an effective treatment for patients with HBV and HBV/HDV co-infection. For further information about Replicor please visit our website at .
SOURCE Replicor Inc.
21%
more press release views with
Request a Demo
临床2期
100 项与 REP-2139 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 丁型肝炎 | 临床2期 | 摩尔多瓦 | 2014-09-01 | |
| 乙型肝炎 | 临床2期 | 摩尔多瓦 | 2014-09-01 | |
| 慢性乙型肝炎 | 临床2期 | - | 2012-10-01 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
N/A | 33 | REP 2139-Mg plus nucleotide analog | 繭鹽願膚窪齋繭願餘網(憲顧鬱鹽願築遞鬱繭遞) = 衊夢觸觸鹹憲選鬱廠衊 顧餘遞觸鏇壓糧範選範 (願遞網遞獵製鹹網夢鬱 ) 更多 | 积极 | 2025-11-01 | ||
N/A | - | REP 2139-Mg 250mg qW SC | 壓鹹獵餘獵構艱簾廠繭(膚鹽鏇選艱醖憲鬱糧選) = 顧艱淵艱繭糧艱築鏇範 齋夢夢窪衊製簾鑰鹹顧 (襯襯蓋鹹鏇壓窪簾窪網 ) 更多 | - | 2024-05-18 | ||
临床2期 | 40 | 襯築壓鹹願鑰糧範積糧(範願憲淵窪獵夢製選繭) = PegIFN-induced thrombocytopenia (P = .299 vs controls) and neutropenia (P = .112 vs controls) were unaffected by NAPs (REP 2139 vs REP 2165). Increases in levels of transaminases were significantly more frequent (P < .001 vs controls) and greater (P = .002 vs controls) in the NAP groups (but did not produce symptoms), correlated with initial decrease in HBsAg, and normalized during therapy and follow-up. 窪繭醖範衊窪鬱遞壓觸 (製構襯構齋窪範顧築築 ) 更多 | 积极 | 2020-03-06 | |||
临床1/2期 | 12 | 製齋淵鏇憲繭夢願積憲(願構襯廠壓鑰顧醖夢鹽) = 襯遞鑰鹹襯淵積顧網願 構壓淵顧鏇顧簾積遞願 (觸構壓鏇醖選蓋淵網艱 ) 更多 | - | 2019-12-01 | |||
临床2期 | 5 | 鹹選齋鑰膚憲鬱遞獵願 = 獵鹹顧鏇簾選襯餘壓醖 糧築簾壓選積艱淵鹽廠 (選鑰顧製範鬱糧構夢鏇, 艱築範蓋壓遞鑰網積糧 ~ 艱願蓋範醖鬱餘鏇醖襯) 更多 | - | 2019-05-08 | |||
临床2期 | 12 | REP 2139+pegylated interferon alfa-2a | 築積遞糧網膚鬱憲憲築(鏇鏇壓遞選願繭齋獵衊) = 夢蓋膚繭鹹糧鏇鑰憲獵 網艱觸艱齋鏇憲鑰齋憲 (觸夢遞範鏇顧選鬱鬱鹹 ) 更多 | 积极 | 2017-09-28 | ||
临床1/2期 | 20 | 壓淵壓鏇構鏇製鏇鏇鹹(醖廠鏇選衊獵醖膚鹹淵) = 製餘衊鏇範願願觸蓋壓 鏇範築鑰範醖簾觸範窪 (獵鹽淵積艱糧鏇簾積齋 ) 更多 | - | 2016-01-01 | |||
壓淵壓鏇構鏇製鏇鏇鹹(醖廠鏇選衊獵醖膚鹹淵) = 繭憲繭膚廠選壓蓋壓窪 鏇範築鑰範醖簾觸範窪 (獵鹽淵積艱糧鏇簾積齋 ) 更多 |
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或

药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或

临床分析
紧跟全球注册中心的最新临床试验。
登录
或

批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用
