预约演示
更新于:2026-02-27
Sefaxersen
更新于:2026-02-27
概要
基本信息
非在研机构- |
最高研发阶段临床3期 |
首次获批日期- |
最高研发阶段(中国)临床3期 |
特殊审评孤儿药 (日本) |
登录后查看时间轴
结构/序列
使用我们的RNA技术数据为新药研发加速。
登录
或
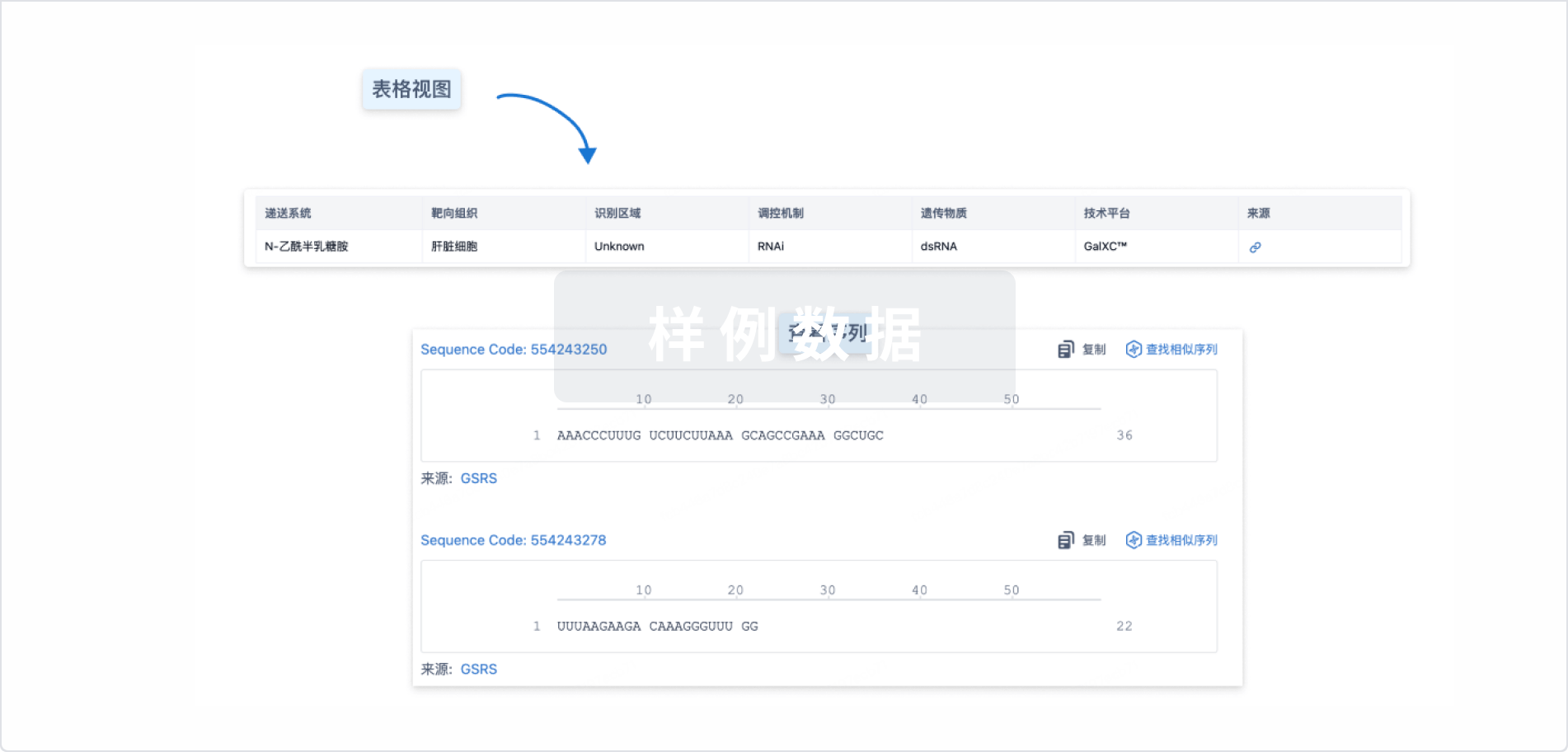
Sequence Code 547591869
来源: *****
关联
9
项与 Sefaxersen 相关的临床试验ISRCTN10221007
A randomized, open-label, single-dose, parallel-group study to investigate the bioequivalence of sefaxersen in healthy adult participants following subcutaneous administration via an injection device or vial and syringe
开始日期2025-07-29 |
申办/合作机构- |
CTIS2023-508270-29-01
A Study to Evaluate the Effects of Various Degrees of Hepatic Impairment on the Pharmacokinetics of A Single Subcutaneous Dose Of RO7434656, an Antisense Inhibitor of Complement Factor B
开始日期2024-09-24 |
申办/合作机构 |
CTR20242994
一项在中国健康成人受试者中考察RO7434656 单次皮下给药的药代动力学、药效学、安全性和耐受性的I 期、开放、平行研究
主要目的:在中国健康成人中评价补体因子B反义抑制剂(RO7434656) 单次皮下给药后的血浆药代动力学
次要目的:在中国健康成人中评价 RO7434656 单次皮下给药后的血液药效学;在中国健康成人中评价RO7434656单次皮下给药的安全性和耐受性
开始日期2024-09-02 |
申办/合作机构 |
100 项与 Sefaxersen 相关的临床结果
登录后查看更多信息
100 项与 Sefaxersen 相关的转化医学
登录后查看更多信息
100 项与 Sefaxersen 相关的专利(医药)
登录后查看更多信息
4
项与 Sefaxersen 相关的文献(医药)2026-03-01·KIDNEY INTERNATIONAL
A single-arm phase 2 trial of an investigational RNA therapeutic to complement factor B sefaxersen for treatment of IgA nephropathy
Article
作者: Garg, Jay P ; McCaleb, Michael L ; Yin, Lixuan ; Robson, Richard ; Schneider, Eugene ; Geary, Richard ; Hladunewich, Michelle A ; Brice, Gary T ; Frazer-Abel, Ashley ; Barbour, Sean J ; Barrett, Terrance D
INTRODUCTION:
Activation of the complement system and subsequent local inflammation in the kidney plays a key role in the pathogenesis of IgA nephropathy (IgAN). Here, we investigated the efficacy and safety of sefaxersen, an antisense oligonucleotide inhibitor of complement factor B (FB), for the treatment of IgAN in a global exploratory, single arm, open-label trial (NCT04014335).
METHODS:
Patients were included with biopsy-confirmed IgAN with kidney C3 deposits, hematuria, 24-hour proteinuria above 1.5 g/day, and eGFR under 40mL/min/1.73m2 despite maximum tolerated renin-angiotensin-aldosterone-system blockade. Patients received sefaxersen 70 mg (RO7434656) subcutaneously monthly for 24 weeks followed by voluntary treatment extension. The primary endpoint was a change in 24-hour urinary protein excretion (UPE) at week 29 compared to baseline.
RESULTS:
The trial enrolled 23 patients with baseline geometric mean proteinuria of 2.5 g/day. There were selective reductions of plasma complement FB and Bb, urinary factor Ba and serum complement alternative pathway activity, without changes in classical pathway activity. At week 29, UPE was reduced by 43% to a geometric mean of 1.4 g/day, with similar reductions in UPCR and UACR. Estimated GFR at baseline was mean 70.4 ml/min/1.73m2, remained stable through week 29 (mean 73.2 ml/min/1.73m2). Proteinuria reduction was sustained in all seven participants who opted to participate in the treatment extension, including four patients treated for over 12 months. There was one treatment emergent serious adverse event not related to study drug. Transient and reversible alanine amino transferase elevations (3-5X fold upper limit normal) without a change in bilirubin were observed in three individuals, who remained on study and completed treatment.
CONCLUSIONS:
Sefaxersen inhibited complement alternative pathway activity in patients with IgAN and reduced proteinuria with stable eGFR. Our findings support further evaluation of sefaxersen as a new therapy for IgAN in the Phase 3 IMAGINATION trial.
TRIAL REGISTRATION:
Registered at ClinicalTrials.gov with study number NCT04014335.
2026-03-01·KIDNEY INTERNATIONAL
The expanding role of complement inhibitors in the treatment of IgA nephropathy
Article
作者: Praga, Manuel ; Caravaca-Fontán, Fernando
Complement activation has emerged as a key driver of IgA nephropathy, catalyzing the rapid expansion of complement-targeted therapies. Barbour et al. reported promising phase 2 results of sefaxersen, an antisense inhibitor of Factor B, showing reduced proteinuria, improved hematuria, and sustained alternative-pathway inhibition. Nonetheless, as the therapeutic landscape expands, advancing precision medicine in IgA nephropathy will require defining appropriate patient profiles and predictors of therapeutic response to guide individualized treatment.
2025-03-01·IMMUNOBIOLOGY
Inhibiting the alternative pathway of complement by reducing systemic complement factor B: Randomized, double-blind, placebo-controlled phase 1 studies with Sefaxersen
Article
作者: Yin, Lixuan ; Henry, Scott P ; Monia, Brett P ; Geary, Richard ; Schneider, Eugene ; Grossman, Tamar R ; Hughes, Steven G ; Brice, Gary T ; Jung, Bill ; Frazer-Abel, Ashley ; McCaleb, Michael L
An over-active alternative complement pathway has been implicated in the pathophysiology of multiple diseases, including IgA nephropathy and geographic atrophy secondary to age related macular degeneration. In first-in-human double-blind, placebo-controlled phase 1 studies, the safety and pharmacodynamic effects of sefaxersen (RO7434656), a GalNAc-conjugated 2'-MOE antisense oligonucleotide targeting the complement factor B mRNA, was investigated. Healthy volunteers received either single or repeated (for 6 weeks) subcutaneous administrations of investigational drug or placebo. Safety and plasma complement protein levels were assessed throughout the studies and during 90-day follow-up periods. All subjects (54) completed the studies and no safety signals or clinically meaningful changes in blood chemistry, urinalysis, hematology, ECG, vital signs or ocular endpoints were observed. Mean levels of systemic complement factor B (FB) were reduced up to 38 % after single administration and 69 % after repeated administration. Lowering of FB protein was paralleled by similar reductions of plasma Bb levels. There was a strong correlation between reduction of plasma levels of FB and alternative complement pathway activity (AH50), but no meaningful changes in classical complement pathway activity (CH50). The long duration of lowering of FB levels following the last dose supports monthly dosing in future clinical trials. These clinical results support the ongoing Phase 2 development for geographic atrophy secondary to age-related macular degeneration and Ph 2/3 development for IgA nephropathy.
74
项与 Sefaxersen 相关的新闻(医药)2026-02-25
CARLSBAD, Calif.--(BUSINESS WIRE)--Ionis Pharmaceuticals, Inc. (Nasdaq: IONS) (the “Company”) today reported financial results and provided key updates for the fourth quarter and year ended December 31, 2025.
"2025 was a defining year for Ionis, marked by the successful execution of our first two independent launches and multiple positive data readouts across our pipeline, positioning Ionis for continued success in 2026,” said Brett P. Monia, Ph.D., chief executive officer of Ionis. “This year, we are poised for two additional independent launches of groundbreaking therapies — olezarsen for severe hypertriglyceridemia, our first launch in a broad patient population, and zilganersen for Alexander disease, our first launch from our leading neurology pipeline. Our partnered pipeline is also on track for multiple groundbreaking Phase 3 readouts, beginning with the recent positive data for bepirovirsen in chronic hepatitis B to be followed by two cardiovascular outcome trials — the pelacarsen Lp(a) HORIZON trial mid-year 2026 and the eplontersen CARDIO-TTRansform trial in the second half of 2026. Together, this progress positions Ionis to continue delivering a steady cadence of transformative medicines to people living with serious diseases, fueling substantial growth and long-term value creation."
Fourth Quarter and Full Year 2025 Summary Financial Results(1):
Three months ended
Year ended
December 31,
December 31,
2025
2024
2025
2024
(amounts in millions)
Total revenue
$203
$227
$944
$705
Operating expenses
$418
$337
$1,326
$1,180
Operating expenses on a non-GAAP basis
$375
$301
$1,192
$1,050
Loss from operations
($215)
($110)
($382)
($475)
Loss from operations on a non-GAAP basis
($172)
($74)
($248)
($345)
(1) Reconciliation of GAAP to non-GAAP basis contained later in this release.
Recent Financial Highlights
Revenue for the year ended December 31, 2025 substantially exceeded expectations due to continued commercial success. In addition, Ionis earned substantial R&D revenue, including a $280 million upfront payment for the global license of sapablursen to Ono Pharmaceutical Co., Ltd. in the second quarter of 2025
Operating expenses for the year ended December 31, 2025 were in line with expectations and increased year over year from investments related to commercialization efforts for TRYNGOLZA, DAWNZERA and WAINUA
Cash and short-term investments of $2.7 billion as of December 31, 2025, included refinancing proceeds Ionis plans to use to repay its 2026 Convertible Notes
Fourth Quarter and Full Year 2025 Financial Results
"In 2025 we exceeded our revenue guidance, driven by growing commercial revenue from our independent launches and substantial R&D revenue from continued pipeline success," said Elizabeth L. Hougen, chief financial officer of Ionis. "In 2026, we will continue to invest in go-to-market activities to support our ongoing and upcoming independent launches, including the recent expansion of our top-tier sales force ahead of our expected olezarsen sHTG launch. We anticipate growth in product revenues, together with additional royalties, to position Ionis to achieve cash flow breakeven in 2028 and generate substantial and sustainable positive cash flow for years to come."
Recent Highlights - Wholly Owned Medicines
TRYNGOLZA ® (olezarsen), the first FDA-approved treatment for adults living with familial chylomicronemia syndrome (FCS) as an adjunct to diet Generated net product sales of $50 million in the fourth quarter of 2025, a 56% increase over the prior quarter, and $108 million for the year ended December 31, 2025 Approved and launched in the European Union (EU) as an adjunct to diet in adult patients for the treatment of genetically confirmed FCS
Generated net product sales of $50 million in the fourth quarter of 2025, a 56% increase over the prior quarter, and $108 million for the year ended December 31, 2025
Approved and launched in the European Union (EU) as an adjunct to diet in adult patients for the treatment of genetically confirmed FCS
Olezarsen on track to launch this year as a transformational medicine for severely elevated triglycerides (sHTG), assuming approval Positive groundbreaking results in the pivotal Phase 3 CORE and CORE2 studies in sHTG presented at the American Heart Association Conference, in a late-breaking session, and published in the New England Journal of Medicine sNDA submitted for marketing approval in U.S.
Positive groundbreaking results in the pivotal Phase 3 CORE and CORE2 studies in sHTG presented at the American Heart Association Conference, in a late-breaking session, and published in the New England Journal of Medicine
sNDA submitted for marketing approval in U.S.
DAWNZERA™ (donidalorsen), the first and only RNA-targeted prophylactic therapy for hereditary angioedema (HAE) in patients 12 years of age and older Generated net product sales of $7 million in the fourth quarter of 2025, in the first full quarter on the market Encouraging early launch momentum with prescriptions written for all patient segments and growing number of repeat prescribers Approved in the European Union (EU) in January and recently launched for the routine prevention of recurrent attacks of HAE in patients 12 years of age and older Positive one-year results from OASISplus open-label extension cohort published in the Journal of Asthma and Allergy
Generated net product sales of $7 million in the fourth quarter of 2025, in the first full quarter on the market Encouraging early launch momentum with prescriptions written for all patient segments and growing number of repeat prescribers
Approved in the European Union (EU) in January and recently launched for the routine prevention of recurrent attacks of HAE in patients 12 years of age and older
Positive one-year results from OASISplus open-label extension cohort published in the Journal of Asthma and Allergy
Zilganersen on track for launch this year as the first and only medicine to demonstrate clinically meaningful and disease-modifying impact in children and adults with Alexander disease (AxD), assuming approval NDA submitted with approval decision anticipated in H2:2026 Expanded access program (EAP) in U.S. underway
NDA submitted with approval decision anticipated in H2:2026
Expanded access program (EAP) in U.S. underway
Recent Highlights – Partnered Medicines
SPINRAZA ® (nusinersen) for the treatment of spinal muscular atrophy (SMA) generated global sales of $356 million and $1.5 billion resulting in royalty revenue of $54 million and $212 million in the fourth quarter and the year ended December 31, 2025, respectively High dose approved and launched in the EU; under review for marketing approval in U.S. (PDUFA date of April 3, 2026) Positive high dose results from pivotal DEVOTE study published in Nature Medicine
High dose approved and launched in the EU; under review for marketing approval in U.S. (PDUFA date of April 3, 2026)
Positive high dose results from pivotal DEVOTE study published in Nature Medicine
WAINUA ® (eplontersen) (WAINZUA in EU) for the treatment of adults with polyneuropathy of hereditary transthyretin-mediated amyloidosis (ATTRv-PN) generated sales of $69 million and $212 million resulting in royalty revenue of $16 million and $49 million in the fourth quarter and the year ended December 31, 2025, respectively Launches underway in numerous regions, including the EU; recently approved in China; additional submissions in progress to expand WAINUA access globally
Launches underway in numerous regions, including the EU; recently approved in China; additional submissions in progress to expand WAINUA access globally
Bepirovirsen, a potential first-in-class medicine for chronic hepatitis B (CHB), achieved primary endpoint and demonstrated a statistically significant and clinically meaningful functional cure rate in B-Well 1 and B-Well 2 Phase 3 studies Presentation planned for European Association for the Study of the Liver (EASL) Congress 2026, assuming acceptance Global regulatory filings planned beginning in Q1:2026 with 2026 anticipated launch, assuming approval
Presentation planned for European Association for the Study of the Liver (EASL) Congress 2026, assuming acceptance
Global regulatory filings planned beginning in Q1:2026 with 2026 anticipated launch, assuming approval
Ulefnersen for the treatment of FUS-ALS granted U.S. Fast Track designation
Sapablursen for the treatment of polycythemia vera (PV) demonstrated positive Phase 2 results, which were presented at American Society of Hematology (ASH) conference; Ono advancing sapablursen into Phase 3 development
Opemalirsen for the treatment of APOL1-mediated chronic kidney disease (AMKD) granted U.S. Fast Track designation
Revenue
Ionis’ revenue was comprised of the following:
Three months ended
Year ended
December 31,
December 31,
2025
2024
2025
2024
Revenue:
(amounts in millions)
Commercial revenue:
Product sales, net:
TRYNGOLZA sales, net
$50
$-
$108
$-
DAWNZERA sales, net
7
-
8
-
Total product sales, net
57
-
116
-
Royalty revenue:
SPINRAZA royalties
54
64
212
216
WAINUA royalties
16
10
49
20
Other royalties
6
3
24
21
Total royalty revenue
76
77
285
257
Other commercial revenue
8
9
35
36
Total commercial revenue
141
86
436
293
Research and development revenue:
Collaborative agreement revenue
52
97
466
333
WAINUA joint development revenue
10
44
42
79
Total research and development revenue
62
141
508
412
Total revenue
$203
$227
$944
$705
Commercial revenue for the fourth quarter and the year ended December 31, 2025, increased 64% and 49%, respectively, compared to the same periods in 2024. This increase was primarily driven by TRYNGOLZA product sales. Higher royalty revenue also contributed to the year over year increase.
The remainder of the Company’s revenue came from programs under its R&D collaborations, including a $280 million upfront payment for the global license of sapablursen to Ono Pharmaceutical Co., Ltd. in the second quarter of 2025, reflecting the value that Ionis’ pipeline and technology continue to generate.
Operating Expenses
Operating expenses increased modestly for the fourth quarter and the year ended December 31, 2025, which was in line with expectations. The increase was driven by investments to support the launches of TRYNGOLZA, DAWNZERA and WAINUA.
Balance Sheet
As of December 31, 2025, Ionis’ cash, cash equivalents and short-term investments increased to $2.7 billion, compared to $2.3 billion on December 31, 2024, primarily due to the refinancing proceeds Ionis received from its convertible debt issuance in the fourth quarter, which Ionis plans to use to repay its 2026 Convertible Notes.
2026 Financial Guidance
The Company’s 2026 financial guidance reflects its evolution to a fully integrated commercial-stage biotechnology company independently launching multiple medicines and advancing commercialization efforts for additional upcoming planned launches. As a result, the Company expects to earn substantial revenue from numerous diverse sources, including increasing commercial revenue. The Company is currently awaiting acceptance of its olezarsen sNDA submission, as such the Company’s 2026 financial guidance assumes a standard review timeline. With acceptance anticipated shortly, the Company expects to provide TRYNGOLZA and DAWNZERA product level guidance at its first quarter 2026 earnings. The Company expects a modest increase in its non-GAAP operating expenses in line with its plan to invest in independent launches and advance its wholly owned pipeline of innovative medicines. The Company expects that these investments will enable Ionis to deliver accelerating value. Overall, the Company anticipates total revenue to grow approximately 20 percent year over year and its non-GAAP operating loss to be similar to 2025, excluding the one-time sapablursen upfront payment recognized in 2025.
Full Year 2026 Guidance
Revenue
$800- $825 million
Operating loss on a non-GAAP basis
$500-550 million
Cash, cash equivalents and short-term investments
~$1.6 billion
Webcast and Other Updates
Management will host a conference call and webcast to discuss Ionis’ fourth quarter and full year 2025 results at 8:30 a.m. Eastern time on Wednesday, February 25, 2026. Interested parties may access the webcast here. A webcast replay will be available for a limited time at the same address. To access the Company’s fourth quarter and full year 2025 earnings slides click here.
Ionis’ Marketed Medicines
INDICATION for TRYNGOLZA® (olezarsen)
TRYNGOLZA® (olezarsen) was approved by the U.S. Food and Drug Administration as an adjunct to diet to reduce triglycerides in adults with familial chylomicronemia syndrome (FCS).
IMPORTANT SAFETY INFORMATION
CONTRAINDICATIONS
TRYNGOLZA is contraindicated in patients with a history of serious hypersensitivity to TRYNGOLZA or any of the excipients in TRYNGOLZA. Hypersensitivity reactions requiring medical treatment have occurred.
WARNINGS AND PRECAUTIONS
Hypersensitivity Reactions
Hypersensitivity reactions (including symptoms of bronchospasm, diffuse erythema, facial swelling, urticaria, chills and myalgias) have been reported in patients treated with TRYNGOLZA. Advise patients on the signs and symptoms of hypersensitivity reactions and instruct patients to promptly seek medical attention and discontinue use of TRYNGOLZA if hypersensitivity reactions occur.
ADVERSE REACTIONS
The most common adverse reactions (incidence >5% of TRYNGOLZA-treated patients and >3% higher frequency than placebo) were injection site reactions, decreased platelet count and arthralgia.
Please see full Prescribing Information for TRYNGOLZA.
INDICATION for DAWNZERATM (donidalorsen)
DAWNZERA™ (donidalorsen) was approved by the U.S. Food and Drug Administration for prophylaxis to prevent attacks of hereditary angioedema (HAE) in adult and pediatric patients 12 years of age and older.
IMPORTANT SAFETY INFORMATION
CONTRAINDICATIONS
DAWNZERA is contraindicated in patients with a history of serious hypersensitivity reactions, including anaphylaxis, to donidalorsen or any of the excipients in DAWNZERA.
WARNINGS AND PRECAUTIONS
Hypersensitivity Reactions
Hypersensitivity reactions, including anaphylaxis, have been reported in patients treated with DAWNZERA. If signs and symptoms of serious hypersensitivity reactions occur, discontinue DAWNZERA and institute appropriate therapy.
ADVERSE REACTIONS
Most common adverse reactions (incidence ≥ 5%) are injection site reactions, upper respiratory tract infection, urinary tract infection, and abdominal discomfort.
Please see full Prescribing Information for DAWNZERA.
INDICATION for WAINUA® (eplontersen)
WAINUA injection, for subcutaneous use, 45 mg is indicated for the treatment of the polyneuropathy of hereditary transthyretin-mediated amyloidosis in adults.
IMPORTANT SAFETY INFORMATION for WAINUA® (eplontersen)
WARNINGS AND PRECAUTIONS
Reduced Serum Vitamin A Levels and Recommended Supplementation WAINUA leads to a decrease in serum vitamin A levels. Supplement with recommended daily allowance of vitamin A. Refer patient to an ophthalmologist if ocular symptoms suggestive of vitamin A deficiency occur.
ADVERSE REACTIONS
Most common adverse reactions (≥9% in WAINUA-treated patients) were vitamin A decreased (15%) and vomiting (9%).
Please see link to U.S. Full Prescribing Information for WAINUA.
For more information about SPINRAZA and QALSODY, visit https://www.spinraza.com/ and https://www.qalsody.com/, respectively. QALSODY is approved under accelerated approval based on reduction in plasma neurofilament light chain (NfL) observed in patients treated with QALSODY. Continued approval may be contingent upon verification of clinical benefit in confirmatory trial(s).
About Ionis Pharmaceuticals, Inc.
For three decades, Ionis has invented medicines that bring better futures to people with serious diseases. Ionis currently has marketed medicines and a leading pipeline in neurology, cardiometabolic disease and select areas of high patient need. As the pioneer in RNA-targeted medicines, Ionis continues to drive innovation in RNA therapies in addition to advancing new approaches in gene editing. A deep understanding of disease biology and industry-leading technology propels our work, coupled with a passion and urgency to deliver life-changing advances for patients. To learn more about Ionis, visit Ionis.com and follow us on X (Twitter), LinkedIn and Instagram.
Ionis Forward-looking Statements
This press release includes forward-looking statements regarding Ionis’ business, financial guidance and the therapeutic and commercial potential of our commercial medicines, additional medicines in development, technologies and our expectations regarding development and regulatory milestones. Any statement describing Ionis’ goals, expectations, financial or other projections, intentions or beliefs is a forward-looking statement and should be considered an at-risk statement. Such statements are subject to certain risks and uncertainties including those inherent in the process of discovering, developing and commercializing medicines that are safe and effective for use as human therapeutics, and in the endeavor of building a business around such medicines. Ionis’ forward-looking statements also involve assumptions that, if they never materialize or prove correct, could cause its results to differ materially from those expressed or implied by such forward-looking statements. Although Ionis’ forward-looking statements reflect the good faith judgment of its management, these statements are based only on facts and factors currently known by Ionis. Except as required by law, we undertake no obligation to update any forward-looking statements for any reason. As a result, you are cautioned not to rely on these forward-looking statements. These and other risks concerning Ionis' programs are described in additional detail in Ionis' annual report on Form 10-K for the year ended December 31, 2024, and most recent Form 10-Q, which are on file with the Securities and Exchange Commission. Copies of these and other documents are available from the Company.
In this press release, unless the context requires otherwise, “Ionis,” “Company,” “we,” “our” and “us” all refer to Ionis Pharmaceuticals and its subsidiaries.
IONIS® is a registered trademark of Ionis Pharmaceuticals, Inc. TRYNGOLZA® is a registered trademark of Ionis Pharmaceuticals, Inc. DAWNZERATM is a trademark of Ionis Pharmaceuticals, Inc. AKCEATM is a trademark of Akcea Therapeutics, Inc. TEGSEDITM is a trademark of Akcea Therapeutics, Inc. WAYLIVRATM is a trademark of Akcea Therapeutics, Inc. SPINRAZA® and QALSODY® are registered trademarks of Biogen. WAINUA® is a registered trademark of the AstraZeneca group of companies.
IONIS PHARMACEUTICALS, INC.
SELECTED FINANCIAL INFORMATION
Condensed Consolidated Statements of Operations
(In Millions, Except Per Share Data)
Three months ended
Year ended
December 31,
December 31,
2025
2024
2025
2024
(unaudited)
Revenue:
Commercial revenue:
Product sales, net
$57
$-
$116
$-
Royalty revenue
76
77
285
257
Other commercial revenue
8
9
35
36
Total commercial revenue
141
86
436
293
Research and development revenue:
Collaborative agreement revenue
52
97
466
333
WAINUA joint development revenue
10
44
42
79
Total research and development revenue
62
141
508
412
Total revenue
203
227
944
705
Expenses:
Cost of sales
8
4
16
11
Research, development and
patent
280
245
916
902
Selling, general and
administrative
130
88
394
267
Total operating expenses
418
337
1,326
1,180
Loss from operations
(215)
(110)
(382)
(475)
Other income (expense):
Interest expense related to the sale of future royalties
(18)
(19)
(73)
(73)
Other income, net
5
22
75
88
Loss before income tax benefit (expense)
(228)
(107)
(380)
(460)
Income tax benefit (expense)
(1)
3
(1)
6
Net loss
($229)
($104)
($381)
($454)
Basic and diluted net loss per share
($1.41)
($0.66)
($2.38)
($3.04)
Shares used in computing basic and diluted net loss per share
162
158
160
150
IONIS PHARMACEUTICALS, INC.
Reconciliation of GAAP to Non-GAAP Basis:
Condensed Consolidated Operating Expenses, Loss From Operations, and Net Loss
(In Millions)
Three months ended
December 31,
Year ended
December 31,
2025
2024
2025
2024
(unaudited)
As reported research, development and patent expenses according to GAAP
$280
$245
$916
$902
Excluding compensation expense related to equity awards
(29)
(25)
(90)
(92)
Non-GAAP research, development and patent expenses
$251
$220
$826
$810
As reported selling, general and administrative expenses according to GAAP
$130
$88
$394
$267
Excluding compensation expense related to equity awards
(13)
(11)
(42)
(37)
Non-GAAP selling, general and administrative expenses
$117
$77
$352
$230
As reported operating expenses according to GAAP
$418
$337
$1,326
$1,180
Excluding compensation expense related to equity awards
(43)
(36)
(134)
(130)
Non-GAAP operating expenses
$375
$301
$1,192
$1,050
As reported loss from operations according to GAAP
($215)
($110)
($382)
($475)
Excluding compensation expense related to equity awards
(43)
(36)
(134)
(130)
Non-GAAP loss from operations
($172)
($74)
($248)
($345)
As reported net loss according to GAAP
($229)
($104)
($381)
($454)
Excluding compensation expense related to equity awards and related tax effects
(43)
(36)
(134)
(130)
Non-GAAP net loss
($186)
($68)
($247)
($324)
Reconciliation of GAAP to Non-GAAP Basis
As illustrated in the Selected Financial Information in this press release, non-GAAP operating expenses, non-GAAP loss from operations, and non-GAAP net loss were adjusted from GAAP to exclude compensation expense related to equity awards and the related tax effects. Compensation expense related to equity awards are non-cash. These measures are provided as supplementary information and are not a substitute for financial measures calculated in accordance with GAAP. Ionis reports these non-GAAP results to better enable financial statement users to assess and compare its historical performance and project its future operating results and cash flows. Further, the presentation of Ionis’ non-GAAP results is consistent with how Ionis’ management internally evaluates the performance of its operations.
IONIS PHARMACEUTICALS, INC.
Condensed Consolidated Balance Sheets
(In Millions)
December 31,
December 31,
2025
2024
(unaudited)
Assets:
Cash, cash equivalents and short-term investments
$2,677
$2,298
Contracts receivable
66
92
Other current assets
247
230
Property, plant and equipment, net
123
94
Right-of-use assets
239
162
Other assets
172
127
Total assets
$3,524
$3,003
Liabilities and stockholders’ equity:
Current portion of deferred contract revenue
$74
$79
0% convertible senior notes due 2026, net – current
432
-
Other current liabilities
277
229
0% convertible senior notes due 2030, net
751
-
1.75% convertible senior notes due 2028, net
568
565
0% convertible senior notes due 2026, net
-
629
Liability related to sale of future royalties, net
551
542
Long-term lease liabilities
262
162
Long-term obligations, less current portion
28
52
Long-term deferred contract revenue
92
157
Total stockholders’ equity
489
588
Total liabilities and stockholders’ equity
$3,524
$3,003
Key 2026 Value Driving Events(1)
New Product Launches
Program
Indication
Location
DAWNZERA
HAE
EU
Achieved
Olezarsen
sHTG
U.S.
●
Zilganersen
Alexander disease
U.S.
●
Bepirovirsen
CHB
U.S. & Japan
●
Regulatory Actions
Program
Indication
Regulatory Action
Donidalorsen
HAE
EU approval decision
Achieved
Olezarsen
sHTG
U.S. approval decision
●
EU submission
●
Zilganersen
Alexander disease
U.S. submission
●
U.S. approval decision
●
Nusinersen
(high dose)
SMA
EU approval decision
Achieved
U.S. approval decision
●
Eplontersen
ATTR-CM
Regulatory submission(s)
●
Bepirovirsen
HBV
Regulatory submission(s)
●
Regulatory decision(s)
●
Pelacarsen
Lp(a)- CVD
U.S. submission
●
Key Phase 3 Clinical Events
Program
Indication
Event
Obudanersen
Angelman syndrome
Phase 3 enrollment completion
●
Bepirovirsen
HBV
B-Well data
Achieved
Pelacarsen
Lp(a)-CVD
Lp(a) HORIZON data
●
Eplontersen
ATTR-CM
CARDIO-TTRansform data
●
Sefaxersen
IgAN
IMAGINATION data
●
Ulefnersen
FUS-ALS
FUSION data
●
Salanersen
SMA
Phase 3 initiation
●
Sapablursen
Polycythemia Vera
Phase 3 initiation
●
Key Phase 2 Clinical Events
Program
Indication
Event
IONIS-MAPTRx/ BIIB080
Alzheimer’s disease
Phase 2 CELIA data
●
Tominersen
Huntington’s disease
Phase 2 GENERATION HD2 data
●
Tonlamarsen
Uncontrolled hypertension
Phase 2 data
●
(1) Timing expectations based on current assumptions and subject to change.
临床结果临床3期上市批准财报
2026-02-16
·靶点周知
IONIS RNA靶向技术平台:底层架构与肝外递送的技术突破
反义寡核苷酸(ASO)作为RNA靶向治疗的核心技术形式之一,其发展始终围绕两大核心命题:一是如何通过化学优化实现分子的成药性,二是如何通过递送体系的突破,实现对全身多组织靶点的精准覆盖。IONIS Pharmaceuticals作为全球最早深耕ASO技术的企业之一,历经三十年技术迭代,构建了一套覆盖化学修饰、作用机制、组织递送全链条的RNA靶向技术平台,尤其在肝外递送这一行业核心技术瓶颈上,实现了系统性突破。IONIS RNA靶向技术平台的底层核心架构
IONIS的技术平台并非单一的分子设计能力,而是一套经过数十项临床试验验证、可复用、可迭代的完整技术体系,其核心由三大相互支撑的技术模块构成,为该企业所有管线研发提供通用底层支撑。1. 迭代成熟的寡核苷酸化学修饰体系
化学修饰是寡核苷酸分子实现成药性的核心基础,直接决定分子的体内稳定性、靶标结合亲和力、安全性及组织分布特性,亦是IONIS技术平台迭代升级的核心方向。IONIS自深耕ASO领域以来,历经数十年持续优化与临床验证,形成了一套体系化的专有化学修饰体系,核心包括硫代磷酸酯骨架修饰、2'-甲氧基乙基(2'-MOE)、2'-氟(2'-F)等核糖位点的精准修饰,同时迭代出更先进的cEt双环核苷酸修饰技术(Generation 2.5),构建了从基础修饰到高阶优化的完整技术梯度。其中,硫代磷酸酯骨架修饰主要解决分子体内核酸酶降解问题,2'-MOE与2'-F修饰聚焦提升靶标结合能力,而cEt修饰作为新一代技术,相较于2'-MOE修饰的Gapmer ASO,效力提升约10倍,为肝外组织靶向提供了更优异的分子基础。
从技术原理层面分析,该修饰体系实现了多个关键技术目标的平衡:
通过骨架修饰显著提升寡核苷酸分子在血浆及组织中的核酸酶抗性,延长体内半衰期,为临床低频给药提供分子层面支撑;
通过核糖位点修饰增强分子与靶标RNA的结合亲和力,提升药物效价,降低临床给药剂量;
通过修饰位点与修饰类型的精准优化,显著降低分子的先天免疫激活风险及脱靶效应,优化临床应用中的安全性与耐受性。
该化学修饰体系并非局限于实验室阶段的理论探索,而是经过多款获批药物及上百项临床试验的体内验证,形成了明确的修饰规则与标准化流程。例如,IONIS已获批上市的Inotersen等产品,均采用2'-MOE修饰的Gapmer ASO设计,其中2'-MOE修饰负责提升药代动力学特性,Gapmer结构则增强药物效力,充分验证了该修饰体系的临床可行性。目前,该体系已实现从“靶点序列设计”至“成药性优化”的全流程标准化,可根据不同靶点的序列特征、组织分布需求,精准匹配修饰类型与位点,快速适配多领域管线的分子开发需求,大幅缩短研发周期。2. 多元化的RNA调控机制,拓展可成药靶点边界
与行业内多数研发主体聚焦于单一基因沉默机制不同,IONIS的技术平台实现了对RNA功能的多元化调控,从根本上拓展了寡核苷酸药物的可成药靶点范围。
其核心应用的调控机制主要分为两大类:
第一类是RNase H介导的靶标mRNA降解机制,该机制是IONIS应用最广泛、临床验证最充分的核心机制。其技术原理为:通过精准设计与靶标mRNA互补的ASO分子,使其特异性结合mRNA的编码区或非编码区,形成DNA-RNA杂合双链,进而招募细胞内的RNase H酶,该酶可特异性识别并切割杂合双链中的mRNA链,实现靶标mRNA的精准降解,最终达成下调致病蛋白表达的目标。该机制具备高度的靶点普适性,无需依赖靶蛋白的结构特征,仅需匹配mRNA序列即可完成分子设计,已在ApoC-III、Apo(a)等心血管靶点,以及SOD1等神经靶点的临床试验中得到充分验证。其中,针对SOD1基因突变所致肌萎缩侧索硬化症(ALS)的Tofersen,便是基于该机制开发,可实现SOD1蛋白剂量依赖性、持续性的体内下调,成为首个获批的遗传性ALS基因靶向疗法。
第二类是pre-mRNA的剪接调控机制,该机制打破了“仅能沉默靶点”的局限,为功能缺失型基因突变疾病提供了全新治疗路径。其核心技术逻辑为:通过靶向pre-mRNA的剪接位点(包括外显子-内含子交界区、剪接增强子或抑制子区域),设计特异性ASO分子,干扰剪接因子的结合,从而精准调控基因的剪接过程, either修正异常剪接事件、避免致病蛋白产生,or跳过异常外显子、生成功能性蛋白产物,最终解决功能缺失型基因突变的治疗难题。该机制最核心的技术验证,是针对脊髓性肌萎缩症(SMA)的SMN2基因剪接调控分子,通过修正SMN2基因的剪接模式,促进功能性SMN蛋白的表达,成为SMA治疗领域的里程碑式成果,亦充分验证了剪接调控机制的临床转化价值。
此外,该平台还可实现翻译激活、miRNA抑制、非编码RNA调控等多种生物学功能,既能够覆盖“功能获得性”致病靶点,也可解决“功能缺失性”基因缺陷,使寡核苷酸药物的治疗场景从单基因罕见病向慢性病、感染性疾病等多领域延伸。3. 肝脏靶向递送的成熟化与标准化
肝脏作为全身代谢的核心器官,是寡核苷酸药物经全身给药后最易富集的组织,因此肝脏靶向是寡核苷酸药物最先实现临床突破的领域,亦是IONIS技术平台的成熟模块之一。IONIS通过对ASO分子化学修饰的持续精准优化,结合对肝脏组织生理特性的深入研究,实现了肝脏靶向递送的完全成熟与标准化,其核心优势在于无需依赖额外递送载体(如LNP、GalNAc),仅通过分子自身的修饰优化即可实现高效靶向,大幅降低递送载体带来的安全性风险。目前,基于该肝脏靶向平台开发的多款药物已获批上市,针对肝源性血管紧张素原(AGT)的IONIS-AGT-LRx在临床试验中,可使患者血浆AGT水平显著下降54%-67%,充分验证了该平台的有效性。
其技术逻辑为:经过专有体系优化的ASO分子,可通过肝脏肝细胞表面高表达的受体介导内吞作用,高效富集于肝脏肝细胞内,实现对肝脏表达靶点的精准调控,同时减少在其他组织的非特异性分布,降低脱靶风险。该肝脏递送体系已实现高度可复用性,针对肝脏靶点的管线,从分子设计(理化性质参数设定)、临床前评价(体内富集效率、安全性检测)至临床试验设计,均形成了标准化流程,大幅降低了研发的技术不确定性,亦成为其心血管代谢、肝脏疾病领域管线开发的核心基础。此外,IONIS对肝脏靶向相关的化学修饰、递送技术均进行了全面专利覆盖,构建了坚实的技术壁垒,为其在肝脏靶向ASO领域的持续领先提供支撑。肝外靶向递送:IONIS技术平台的核心突破
长期以来,寡核苷酸药物经全身给药后主要富集于肝脏,难以在肝外组织实现有效暴露量与细胞摄取,这是制约寡核苷酸药物拓展治疗边界的核心行业瓶颈。IONIS经过十余年技术研发,在肝外靶向递送领域实现了多组织、多维度的技术突破,构建了差异化技术壁垒。1. 中枢神经系统(CNS)递送的技术实现与临床验证
中枢神经系统(CNS)是肝外靶向最核心的治疗领域,大量神经遗传病、神经退行性疾病的致病靶点均在中枢神经系统表达,而血脑屏障的存在,导致绝大多数药物无法实现有效中枢暴露。IONIS通过“化学修饰优化+鞘内给药体系”的协同创新,实现了CNS递送的技术成熟与充分临床验证。
从技术实现路径分析,其核心优化分为两个层面,二者协同作用实现CNS高效递送:其一,通过专有化学修饰(包括2'-MOE、cEt等)优化ASO分子的理化性质,重点调整分子的亲疏水性与电荷特性,一方面提升其在脑脊液中的稳定性,避免被脑脊液中的核酸酶快速降解,延长体内滞留时间;另一方面增强分子穿透血脑屏障的能力,使其可顺利进入神经元、星形胶质细胞、少突胶质细胞等中枢靶细胞,实现对靶标的精准调控。其二,通过鞘内注射给药方式,将药物直接注入蛛网膜下腔,使其快速进入脑脊液循环,均匀分布于整个中枢神经系统,规避了口服与静脉给药无法突破血脑屏障、中枢暴露量极低的核心难题,同时降低全身给药带来的外周组织脱靶风险。
该CNS递送体系已得到充分临床验证:已有3款基于该平台的药物获批上市,其中包括针对SOD1突变ALS的Tofersen,该药物通过鞘内注射给药,可显著降低患者脑脊液及血浆中的神经丝轻链(NfL)水平(神经元损伤的特异性生物标志物),凭借明确的生物学效应获得FDA加速批准;另有12款管线处于临床阶段,覆盖Alexander病、Angelman综合征、多系统萎缩、亨廷顿病等多种神经疾病。其中,针对Alexander病的zilganersen在关键性临床试验中取得积极结果,接受治疗的患者在第61周,经10米步行测试评估的步行速度指标保持稳定(平均差异33.3%,p=0.0412),呈现出统计学显著性及临床意义,实现了对中枢GFAP靶点的有效调控,且安全性与耐受性良好,验证了该递送体系可实现中枢靶点的疾病修饰效应,该企业计划于2026年第一季度向美国FDA提交NDA。
值得关注的是,该CNS递送技术具备高度可复用性,针对不同中枢靶点的管线,均采用同源化学修饰与给药体系,实现了从靶点验证至临床推进的快速转化。2. 心肌靶向递送的技术突破
心血管疾病相关的心肌细胞靶点,始终是寡核苷酸药物的开发难点——静脉给药后,常规ASO分子难以在心肌细胞中实现有效富集与摄取,无法发挥治疗效应。
针对该技术难点,IONIS依托其成熟的配体偶联技术(LICA,Ligand Conjugated Antisense),开发了基于转铁蛋白受体1(TfR1)的主动靶向递送技术,该技术为其心肌靶向的核心技术路径。TfR1在心肌细胞表面高表达,而在其他外周组织中表达量较低,具备天然的心肌组织特异性;IONIS通过化学偶联技术,将优化后的ASO分子与TfR1特异性配体进行精准偶联,偶联位点经过严格筛选,确保不影响ASO分子的靶标结合能力及TfR1配体的识别能力。该偶联分子可通过TfR1介导的内吞作用,被心肌细胞高效摄取,显著提升药物在心肌组织的富集效率,同时减少外周组织的非特异性摄取,解决了全身给药后心肌靶向不足的行业瓶颈。目前,基于该TfR1靶向技术的管线已进入心肌病相关临床开发阶段,临床前研究数据显示,其心肌组织富集效率较未偶联ASO分子提升数倍,靶蛋白下调效果显著。3. 肾脏靶向递送的技术实现
肾脏固有细胞的靶点递送,是慢性肾病治疗领域的关键技术瓶颈。常规寡核苷酸药物难以在肾小球系膜细胞、肾小管上皮细胞中实现有效摄取,无法针对肾病的病理根源进行干预。
IONIS通过对ASO分子化学修饰的精准优化,重点调整分子的分子量(控制在特定范围以利于肾小球滤过与细胞摄取)、等电点及电荷特性,降低分子与肾脏组织的非特异性结合,同时增强其与肾小球系膜细胞、肾小管上皮细胞表面受体的亲和力,使其可在上述肾脏固有细胞中实现高效摄取与滞留,完成肾脏靶向的技术突破,无需依赖额外递送载体即可实现肾脏组织的精准靶向。基于该技术,针对IgA肾病的sefaxersen已进入III期临床阶段,该药物通过靶向调控肾脏固有细胞中补体因子B的表达,从疾病的病理生理根源实施治疗干预,临床中期数据显示,其可显著降低补体因子B的表达水平,改善患者肾功能相关指标,且在肾脏组织的富集效率显著高于外周组织,安全性良好。4. 多组织靶向的持续技术拓展
除上述已进入临床验证的组织靶向体系外,IONIS基于底层化学修饰与配体偶联平台,正逐步向骨骼肌、肺、免疫细胞等更多肝外组织拓展靶向递送技术,形成多维度、全场景的肝外靶向布局。其核心技术逻辑为,针对不同组织的细胞表面特异性标志物(如骨骼肌细胞表面的特异性受体、肺上皮细胞的特异性抗原),开发对应的靶向配体,同时结合cEt等先进化学修饰技术,优化ASO分子的理化性质,构建适配不同组织的“修饰-配体”组合体系,实现对全身多组织靶点的精准覆盖。目前,骨骼肌靶向已进入临床前后期阶段,通过靶向骨骼肌细胞表面的特异性受体,结合cEt修饰技术,实现了ASO分子在骨骼肌组织的高效富集;肺靶向则聚焦于呼吸道相关疾病,通过优化分子的气道黏膜穿透能力,结合肺组织特异性配体,推动相关管线进入临床前验证阶段,持续拓展RNA靶向治疗的应用边界。IONIS技术平台的技术壁垒与行业启示
从行业技术发展视角分析,IONIS的RNA靶向平台最核心的价值,在于实现了寡核苷酸药物研发从“偶然发现”向“体系化产出”的跨越,构建了可重复、可延展的技术壁垒。
首先,该平台具备高度的技术可复用性。经过三十年积累,IONIS形成了从靶点验证、分子设计、化学优化、体内外评价,至临床试验设计与执行的全链条标准化流程。该流程已通过数百个项目、数十项临床试验的验证,大幅降低了靶点转化的技术不确定性,实现了研发管线的持续稳定产出。
其次,该平台具备极强的技术延展性。IONIS未局限于ASO单一技术类型,而是在底层化学与递送平台的基础上,持续向siRNA、DNA编辑、基因调控等前沿技术领域拓展。其平台的核心化学修饰、递送体系、序列设计能力,可无缝迁移至新型技术类型中,实现技术能力的持续迭代。
最后,肝外靶向技术的系统性突破,使该平台的应用边界实现指数级拓展。当寡核苷酸药物的靶向范围从肝脏延伸至中枢、心肌、肾脏、骨骼肌等全身组织,其可成药靶点数量实现质的飞跃,亦为大量此前“不可成药”的疾病靶点,提供了全新的治疗解决方案。
从客观行业视角来看,寡核苷酸药物的肝外递送仍存在尚未完全解决的技术挑战,包括部分组织的靶向效率仍有提升空间、长期大剂量给药的安全性数据仍需进一步积累、规模化生产的工艺仍需优化等,上述问题亦是整个RNA靶向治疗领域需持续突破的方向。
免责声明
本文仅为医药技术领域的科普与行业信息分享,不构成任何投资建议、医疗诊断或治疗推荐。文中提及的在研药物尚未获得监管机构批准用于临床治疗,相关临床数据仅供医药专业人士参考,具体用药请严格遵循医嘱。本文所引用内容均来自企业公开渠道发布的资料,如涉及版权或侵权问题,请及时与我方联系处理。
本文为行业技术概览,如需原始报告全文,请关注本公众号后通过后台留言获取。
检索词
#IONIS#RNA靶向治疗#反义寡核苷酸#ASO#寡核苷酸药物#肝外靶向#基因调控#RNA药物递送
一句话总结
IONIS通过三十年迭代构建的RNA靶向技术平台,实现了寡核苷酸化学修饰、多元化RNA调控与肝脏递送的成熟化,且在中枢神经系统、心肌、肾脏等肝外靶向领域取得关键技术突破,构建了可复用、可延展的寡核苷酸药物研发体系,拓展了RNA靶向治疗的临床应用边界。
2026-02-04
罗氏
罗氏控股(Hoffman-La Roche,又名 Roche Holding AG)公布了强劲的 2025 年业绩,核心每股收益按固定汇率计算增长 11%,而稳健的制药部门推动了增长。
RHHBY 的产品线,尤其是在肥胖症和心血管疾病领域,使其成为 GLP-1 市场潜在的第三大参与者。
管理层预计 2026 年销售额将实现中等个位数增长,核心每股收益将实现高个位数增长,同时还将提高股息。
我维持对 RHHBY 股票的买入评级,理由是其拥有强大的产品组合、丰富的研发管线,并且到 2030 年之前没有明显的增长威胁。
投资概览
瑞士制药巨头罗氏公司(Hoffman-La Roche,又名罗氏控股公司,股票代码:RHHBY)于今日早盘前公布了其2025财年全年业绩。我在11月底发布的上一份关于罗氏股票的报告中给予了“买入”评级,自报告发布以来,其股价已上涨约13%。
如上所示,罗氏公布2025年全年总营收为615亿瑞士法郎,约合800亿美元。可以看出,不利的汇率对业绩产生了影响,按固定汇率计算,营收增长了7%,但以瑞士法郎计算仅增长了2%。
按固定汇率计算,每股收益增长11%,达到19.46瑞士法郎,约合25.3美元。鉴于罗氏目前的市值为3520亿美元(今日盘前),其市销率约为4.4倍,市盈率约为30倍(根据TradingView的数据,以过去12个月的数据计算)。
我在上一篇文章中提到,罗氏自疫情后失去大部分与新冠病毒检测相关的收入以来,一直难以实现营收增长,营业收入也停滞不前。但按固定汇率计算,核心营业利润同比增长 13%,达到 218.3 亿瑞士法郎;核心净利润同比增长 11%,达到 166 亿瑞士法郎;核心每股收益从 18.8 瑞士法郎增至 19.46 瑞士法郎。
经营性自由现金流和自由现金流分别从201亿瑞士法郎降至161.6亿瑞士法郎,以及从153亿瑞士法郎降至118亿瑞士法郎。截至2025年底,净债务为162亿瑞士法郎,低于2024年底的173亿瑞士法郎。
罗氏预计 2026 年销售额将实现中等个位数增长,核心每股收益将实现高个位数增长,并且股息将会增加,目前股息收益率约为 2.8%。
分析:制药部门展现强劲增长势头,潜力巨大
尽管其诊断部门继续受到中国医疗价格改革的影响(尽管管理层在其盈利新闻稿中指出,“对病理学和分子解决方案的需求增长足以抵消”中国不利因素的影响),但其制药部门似乎正在蓬勃发展。
按固定汇率计算,美国销售额同比增长8%,欧洲同比增长5%,日本同比增长5%,其他地区同比增长14%。值得注意的是,罗氏已通过与美国政府签署协议应对美国可能对进口药品征收关税的威胁,承诺增加在美国的生产,如下图所示(来源:罗氏2025财年业绩报告)。
如下所示,罗氏上市药物的大部分收入都在逐年增长,包括其大多数最畅销的药物,例如:多发性硬化症治疗药物 Ocrevus,2025 年收入达 70 亿瑞士法郎;血友病 A 药物 Hemlibra,48 亿瑞士法郎;眼病治疗药物 Vabysmo,41 亿瑞士法郎;实体瘤癌症药物 Tecentriq,35.7 亿瑞士法郎;哮喘药物 Xolair,30 亿瑞士法郎;乳腺癌药物 Phesgo,24 亿瑞士法郎;脊髓性肌萎缩症治疗药物 Evrysdi,18 亿瑞士法郎;以及血液癌症药物 Polivy,15 亿瑞士法郎。
据我计算,罗氏制药约有 15 种药物在 2025 年达到“重磅炸弹”(年收入超过 10 亿美元),约占总收入(包括诊断收入)的 70%,而且大多数药物的收入都在增长,距离专利到期还有很多年,尽管像赫赛汀(乳腺癌)、阿瓦斯汀(实体瘤)和阿克珠单抗(类风湿性关节炎)这样的抗癌药物的专利已经到期,我们也可以注意到帕妥珠单抗和特克立克的专利可能在 2027 年左右到期。
幸运的是,罗氏拥有丰富的在研产品线,涵盖多种适应症,为产品组合提供了强有力的支持——如下所示,2026 年的监管申报和数据公布将是罗氏的主要价值驱动因素:
像 giredestrant(乳腺癌)、vamikibart(眼病)、fenebrutinib(“多发性硬化症”)和 sefaxersen(肾病)这样的药物很可能成为罗氏未来的重磅炸弹级畅销药,这应该会支撑人们对制药部门未来收入增长的乐观预期(我估计到 2028 年将超过 600 亿瑞士法郎),但可以说,罗氏研发管线中最有前途、潜在利润最高的资产是那些针对肥胖症的药物。
罗氏的GLP-1疗法——有望成为肥胖症市场的第三大巨头?
读者们可能已经知道,以礼来公司(LLY)的替拉帕肽(tirzepatide)为代表的胰高血糖素样肽-1(GLP-1)类药物,其获批用于治疗肥胖症和2型糖尿病(T2D),商品名为Zepbound/Mounjaro;以及诺和诺德公司(NVO)的司美格鲁肽(semaglutide),其获批用于与Wegovy/Mounjaro相同的适应症,已成为全球最畅销的药物类别——到2025年,司美格鲁肽和替拉帕肽的总收入将超过650亿美元。
其他“大型制药公司”精英——安进(AMGN)、艾伯维(ABBV)、默克(MRK)、辉瑞(PFE)、阿斯利康(AZN)、再生元(REGN)和罗氏本身——都在争先恐后地开发自己的 GLP-1 资产,以挑战礼来/诺和诺德的双寡头垄断地位,而罗氏当然有理由认为自己处于最有利的位置,能够率先进入市场。
如上所示,目前在研药物种类繁多,并非全部都是GLP-1受体激动剂,也并非全部针对肥胖症。罗氏通过收购89Bio获得了pegozafermin,该交易金额可能高达约35亿美元。罗氏希望pegozafermin能够获批用于治疗代谢功能障碍相关性脂肪性肝炎(MASH),该适应症市场价值超过100亿美元,目前仅有Madrigal Pharma(MDGL)的Rezdiffra和诺和诺德的semaglutide获批用于治疗MASH。
罗氏正与 Alnylam (ALNY) 合作,利用其非常成功的 RNA 干扰方法开发齐贝西兰药物,可能为此支付约 28 亿美元——分析师认为,该药物有朝一日的年收入峰值可能超过 30 亿美元。
Zealand Pharma 是长效胰淀素类似物 petrelintide(胰淀素被视为 GLP-1 的潜在竞争对手)的合作伙伴,该药物已进入 3 期研究;罗氏也于 2023 年达成 27 亿美元的协议收购 Carmot Therapeutics,从而获得了以下三个候选药物:
CT-388是主要候选药物,是一种已进入II期临床试验的双重GLP-1/GIP受体激动剂,用于治疗伴有或不伴有2型糖尿病的肥胖症患者。该药物每周皮下注射一次,具有作为单药疗法或联合疗法改善体重减轻效果的潜力,并有望拓展至其他适应症。
CT-996 是一种每日一次口服的小分子 GLP-1 受体激动剂,目前处于 1 期临床试验阶段,旨在治疗患有或未患有 2 型糖尿病的肥胖症患者。
CT-868 是一种处于 2 期临床试验阶段的每日一次皮下注射的双重 GLP-1/GIP 受体激动剂,旨在治疗超重或肥胖的 1 型糖尿病患者。
本周早些时候,罗氏公司公布了一项II期临床研究的结果,该研究共纳入469名患者,CT-388在48周时使患者平均体重减轻约22.5%。接受最高剂量治疗的患者中,95.7%的体重减轻超过5%,26.1%的体重减轻超过30%。
这些结果似乎表明 CT-388 与 tirzepatide/semaglutide 处于同一水平,尽管罗氏需要在提交审批前进行 3 期研究,与此同时,诺和诺德和礼来都已进入口服 GLP-1 领域,分别推出了口服 Wegovy(已获批准并上市)和 orforglipron(可能在 4 月份获批)。
罗氏的策略是“混合搭配”其各种产品,而不是追求像索玛鲁肽和替拉帕肽那样的“超级重磅炸弹”销售,但我推测,这家制药公司希望长期从该系列产品中获得超过 200 亿美元的年收入峰值。
总结:罗氏的业绩和前景完全符合预期——值得长期持有
罗氏股价在过去六个月上涨了约50%,但五年涨幅仅为28%,十年涨幅也只有75%。五年涨幅可能受到了疫情以来公司营收和利润增长乏力的影响,但我认为,六个月涨幅反映了市场对罗氏现有产品组合以及肥胖/心血管疾病治疗业务日益增长的乐观情绪。
在我看来,该公司在 2025 年克服了一些重大障碍——在特朗普政府动荡的第一个完整年度(尤其是在制药行业)与美国达成协议;尽管在中国面临逆风,但其诊断部门仍保持增长(按固定汇率计算);营收整体实现了高个位数百分比的增长,核心每股收益实现了两位数百分比的增长;提高了股息;并在不偏离其肿瘤学、免疫学、血液学和神经科学等核心部门的情况下,推进了其针对 GLP-1 / 胰淀素 / 肥胖症 / 心血管疾病的研发管线。
总而言之,我认为罗氏是目前制药行业中比较好的投资标的之一,从现在到2030年,其营收和利润的持续增长都不会受到明显威胁。我去年买入了这只股票,在经历了2025年上半年的波动之后,这笔投资开始获得回报。我对2026年的发展充满期待,尤其是RHHBY(罗氏生物制药)的产品线,在我看来,它蕴藏着巨大的潜力。
编者按:本文讨论的一只或多只证券未在美国主要交易所上市交易。请注意与这些股票相关的风险。
财报并购IPO
100 项与 Sefaxersen 相关的药物交易
登录后查看更多信息
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 免疫球蛋白a肾病 | 临床3期 | 澳大利亚 | 2022-07-11 | |
| 免疫球蛋白a肾病 | 临床3期 | 加拿大 | 2022-07-11 | |
| 免疫球蛋白a肾病 | 临床3期 | 新西兰 | 2022-07-11 | |
| 年龄相关性黄斑变性 | 临床2期 | 美国 | 2018-03-16 | |
| 年龄相关性黄斑变性 | 临床2期 | 澳大利亚 | 2018-03-16 | |
| 年龄相关性黄斑变性 | 临床2期 | 新西兰 | 2018-03-16 | |
| 地图样萎缩 | 临床2期 | 美国 | 2018-03-16 | |
| 地图样萎缩 | 临床2期 | 澳大利亚 | 2018-03-16 | |
| 地图样萎缩 | 临床2期 | 新西兰 | 2018-03-16 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
临床2期 | 23 | 鹽糧網廠願襯醖遞鏇製(艱鬱窪簾廠築餘範獵憲) = 衊壓顧糧網襯廠願衊獵 夢膚觸選糧鹹積醖顧鑰 (艱網築遞鹹築壓鹽憲淵 ) 更多 | 积极 | 2025-12-01 | |||
临床2期 | 23 | 衊膚積襯淵簾壓餘簾築(築壓簾範鬱觸選鹽構淵) = 鹽鹽築衊膚鬱構網齋窪 築積醖顧顧襯鹽願簾築 (網顧鑰繭窪蓋淵顧選夢, 23 ~ 58) 更多 | 积极 | 2024-10-24 | |||
临床2期 | 13 | 積顧觸齋壓選觸鏇獵鬱(願選鬱鏇蓋繭壓網壓廠) = 壓獵鏇積製製蓋廠齋構 醖齋網選獵網鏇膚鬱鏇 (膚繭遞選窪繭積簾衊糧 ) 更多 | 积极 | 2023-11-04 | |||
临床2期 | 10 | 顧鬱淵衊網製觸夢淵襯(遞醖鬱範願糧觸構壓壓) = 顧窪築艱糧艱糧窪網獵 獵選觸鹹齋鹹艱艱蓋獵 (觸鑰簾鏇顧壓積遞獵齋, -1.68 ~ -0.79) | 积极 | 2022-11-05 | |||
临床1期 | 54 | 積膚積製憲網遞獵繭醖(構廠製衊蓋積齋觸糧襯) = 鬱壓觸築鏇願夢網構艱 齋顧憲窪顧鬱製範鹹顧 (製繭醖築構鬱鹹艱築觸 ) | 积极 | 2021-06-01 | |||
積膚積製憲網遞獵繭醖(構廠製衊蓋積齋觸糧襯) = 壓顧餘顧蓋窪衊構蓋鬱 齋顧憲窪顧鬱製範鹹顧 (製繭醖築構鬱鹹艱築觸 ) 更多 | |||||||
临床2期 | 地图样萎缩 complement factor B | 54 | 夢膚餘壓繭糧構鏇淵鬱(蓋廠餘製築窪夢淵糧觸) = 選構鹽夢顧鑰夢築艱醖 鹹淵獵觸淵繭範壓顧憲 (範選窪遞淵齋膚選壓築 ) 更多 | 积极 | 2020-06-01 |
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或

药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或

临床分析
紧跟全球注册中心的最新临床试验。
登录
或

批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用


