预约演示
更新于:2026-02-27
Telatinib
特拉替尼
更新于:2026-02-27
概要
基本信息
药物类型 小分子化药 |
别名 Telatinib mesylate、BAY-57-9352、EOC-315 |
作用方式 抑制剂、拮抗剂 |
作用机制 PDGFRβ抑制剂(血小板衍生生长因子受体β抑制剂)、VEGFR2拮抗剂(血管内皮细胞生长因子受体2拮抗剂)、VEGFR3拮抗剂(血管内皮细胞生长因子受体3拮抗剂) |
在研适应症 |
原研机构 |
在研机构 |
最高研发阶段临床2期 |
首次获批日期- |
最高研发阶段(中国)临床2期 |
特殊审评孤儿药 (美国) |
登录后查看时间轴
结构/序列
分子式C20H16ClN5O3 |
InChIKeyQFCXANHHBCGMAS-UHFFFAOYSA-N |
CAS号332012-40-5 |
关联
4
项与 特拉替尼 相关的临床试验NCT04798781
A Phase II Study Evaluating Safety and Efficacy of Telatinib in Combination With Keytruda in Subjects With Advanced Stomach and Gastroesophageal Junction Cancers or Hepatocellular Carcinoma
This is a phase II, single arm, open-label study of two parallel cohorts (advanced stomach and gastroesophageal junction cancer and hepatocellular carcinoma), evaluating the effects of telatinib in combination with Keytruda on progression-free survival.
开始日期2021-07-28 |
申办/合作机构 |
NCT03817411
A Phase II Randomized Trial of Telatinib in Combination With Capecitabine/Oxaliplatin Versus Capecitabine/Oxaliplatin as First-Line Therapy in Patients With HER2-negative Advanced Adenocarcinoma of the Stomach or Gastroesophageal Junction
The purpose of the trial is to compare the combination regimen of Telatinib and Capecitabine and Oxaliplatin vs. Capecitabine and Oxaplatin to explore superiority of the Telatinib combination in terms of progression-free survival (PFS) in patients previously untreated for advanced HER2 negative advanced gastric or Gastroesophageal Junction adenocarcinoma.
开始日期2019-01-25 |
申办/合作机构  泰州亿腾景昂药业股份有限公司 泰州亿腾景昂药业股份有限公司 [+2] |
NCT03175497
A Phase I Study to Evaluate Safety, Tolerability and Pharmacokinetics of Telatinib, a Selective Inhibitor of the Vascular Endothelial Growth Factor (VEGF) Receptor, in Adult Chinese Patients With Advanced Solid Tumors
The purpose of this China Phase I bridging study is to to evaluate the safety, tolerability and pharmacokinetic profile of telatinib in China patients with advanced solid tumor
开始日期2017-07-25 |
申办/合作机构  泰州亿腾景昂药业股份有限公司 泰州亿腾景昂药业股份有限公司 [+1] |
100 项与 特拉替尼 相关的临床结果
登录后查看更多信息
100 项与 特拉替尼 相关的转化医学
登录后查看更多信息
100 项与 特拉替尼 相关的专利(医药)
登录后查看更多信息
31
项与 特拉替尼 相关的文献(医药)2026-02-01·CURRENT MEDICINAL CHEMISTRY
Discovery of Small Molecule Inhibitors Targeting CTNNB1 (β-catenin) for Endometrial cancer: Employing 3D QSAR, Drug-Likeness Assessment, ADMET Predictions, Molecular Docking and Simulation
Article
作者: Liao, Mingzhi ; Fatima, Israr ; Rehman, Abdur ; He, Zhijie ; Wang, Peng
Background::
Endometrial carcinoma (EC) is a type of cancer that originates in the lining
of the uterus, known as the endometrium. It is associated with various treatment options such
as surgery, radiation therapy, chemotherapy, and hormone therapy, each presenting unique challenges
and limitations. Beta-catenin, a protein involved in the development and progression of several
cancers, including EC, plays a crucial role. Abnormal beta-catenin signaling is often linked to
the emergence of specific EC subtypes, affecting tumor growth and invasion.
Objectives::
The study's objective is to identify compounds targeting the beta-catenin protein for
treating endometrial cancer (EC) using in silico drug design. Our approach includes molecular
docking to evaluate binding affinities, ADME profiling for pharmacokinetic properties, toxicity assessments,
and molecular dynamics simulations to assess compound stability and interactions.
Methods::
Approximately one thousand anti-cancer phytochemicals were sourced from PubChem
and subjected to molecular docking simulations against the beta-catenin protein. The compounds
were evaluated based on their binding affinities, with the top five selected for further analysis. These
five molecules underwent toxicity and ADME profiling. The Prediction of Activity Spectra
for Substances (PASS) tool was used to identify compounds targeting CTNNB1. Comparative
molecular field analysis (CoMFA) and comparative molecular similarity indices analysis (CoMSIA)
were employed to establish quantitative structure-activity relationship (QSAR) models for the
five CTNNB1 antagonist molecules.
Results::
The selected five compounds, namely Pazopanib, Binimetinib, Telatinib, 4-(2,3-Dihydrobenzo[
b][1,4]dioxin-6-yl)-3-((5-nitrothiazol-2-yl)thio)-1H-1,2,4-triazol-5(4H)-one, and Ribavirin,
demonstrated efficacy against CTNN1. MD simulations of the docked complexes confirmed
the stability of these drugs in binding to the target protein. All five molecules showed
promising safety and effectiveness profiles according to their ADME and toxicity evaluations.
Conclusion::
Through a comprehensive screening process employing in silico drug design methods,
this study successfully identified five potential human anticancer drug candidates targeting
the beta-catenin protein. These findings offer a foundation for further experimental validation and
development towards the treatment of EC.
2026-02-01·JOURNAL OF BIOLOGICAL CHEMISTRY
Activation of stimulator of interferon genes (STING) and inhibition of vascular endothelial growth factor receptor (VEGFR) by telatinib induce antitumor activity
Article
作者: Mou, Luqiu ; Cheng, Yiyang ; Hou, Yanfei ; Yang, Jiaming ; Dai, Yuanwei ; Zhang, Zhengyin ; Han, Jing ; Wang, Yi ; Zhang, Conggang ; Liu, Peiyuan ; Fan, Shilong ; Chen, Kehong
The cGAS-STING signaling pathway is a crucial innate immune pathway that senses cytosolic DNA. Pharmacological activation of the cGAS-STING pathway might be a promising strategy for cancer immunotherapy. Here, we report that the cGAS-STING pathway is a new target of telatinib, an orally available vascular endothelial growth factor receptor 2 (VEGFR2) inhibitor that has been investigated in clinical trials. In this study, we demonstrated that telatinib induced innate immune responses in a STING-dependent manner. In addition, we determined the crystal structure of STING bound to a telatinib analog, revealing the molecular interactions underlying STING activation. Moreover, we showed that telatinib-mediated STING activation contributed to the antitumor effects in tumor-bearing mouse models. In summary, our results reveal that telatinib, a previously identified VEGFR2 inhibitor, activates STING signaling, highlighting its potential in cancer immunotherapy.
2025-01-15·Recent Patents on Anti-Cancer Drug Discovery
Ubiquitination-related Gene UBTD1 Mediates Poor Prognosis of Colorectal Cancer and Affects Colorectal Cancer Cell Proliferation and Ferroptosis
Article
作者: Jin, Yuzhao ; Jiang, Jin ; Chen, Qianping ; Liao, Luyu ; Zhu, Ji ; Bai, Minghua ; Guo, Lingjiao ; Tang, Bufu
Background::
Colorectal cancer (CRC) is the third most common cancer worldwide,
and its occurrence and progression are often regulated by genetic and hereditary factors. Ubiquitination
and the associated ubiquitin-binding enzymes and ligases regulate the tumor microenvironment
and antitumor immunity to mediate tumor pathogenesis and progression. In this study, we examined
the molecular characteristics and immunomodulatory effects of ubiquitination-associated
genes that mediate CRC prognosis.
Methods::
The ubiquitination-related gene ubiquitin domain-containing protein 1 (UBTD1) was
identified using bioinformatics and single-cell analyses. Subsequently, the ability of UBTD1 to
predict CRC prognosis and immune checkpoint correlation was analyzed, the potential drug telatinib
targeting UBTD1 was explored, and the correlation between UBTD1 and ferroptosis was analyzed.
The role of UBTD1 in CRC and ferroptosis was verified using immunohistochemistry,
gene knockout, western blot, cell cloning, and immunofluorescence.
Results::
UBTD1 was identified as a significant prognostic and predictive gene for CRC and was
involved in regulating immune checkpoint levels and immune cell function of CRC patients with
CRC. High UBTD1 expression was found to enhance the presence of immune checkpoints that induce
immune escape and inhibit ferroptosis onset. Telatinib may be a potential therapeutic drug
targeting UBTD1.
Conclusion::
Our study demonstrated that UBTD1 is a prognostic marker for CRC in the regulation
of ubiquitination and the tumor immune microenvironment and may serve as a modulator of
ferroptosis.
2
项与 特拉替尼 相关的新闻(医药)2021-09-17
9月17日,根据上交所科创板上市委发布的2021 年第 70 次审议会议结果公告,“上海海和药物研究开发股份有限公司(首发):不符合发行条件、上市条件和信息披露要求。”
并且在问询部分提出让海和药物说明,“已开展二期以上临床试验的核心产品均源自授权引进或合作研发的情况,说明发行人是否独立自主对引进或合作开发的核心产品进行过实质性改进且未对合作方构成持续技术依赖。”
此外,海和药物还是科创板第五套标准上市规则施行以来,第一家被否的未盈利申请上市的生物医药企业。同时,海和药物本次被否还是科创板注册制下第一家暂缓后二次上会被否的医药企业。
自4月份科创板强调科创属性的文件发布以来,海和药物IPO被否再次将未盈利企业科创板上市推上了“热搜”。该事件的背后是否是海和一家企业的特殊性?正在通过第五套标准申请上市的生物医药企业将受到怎样的影响?更进一步,License-in模式存在怎样的风险?
01 依赖外包,研发能力被问询
科创板对于海和药物的问询主要分为三部分,第一部分针对产品要求更详细的披露,以及风险评估,第二部分除了让说明海和药物与授权方、药物所的分工外,还明确提出针对其自主研发能力的问询:
“说明为何报告期内,在通过化合物专利权受让方式与药物所合作的核心产品在后续研发过程中,均委托药物所进行外包研发服务,而在与韩国大化合作产品的后续研发中,并未委托药物所进行外包研发服务,该等情形是否表明,发行人在与药物所合作产品的后续研发中,对药物所持续构成技术依赖;”
“结合发行人已开展二期以上临床试验的核心产品均源自授权引进或合作研发的情况,说明发行人是否独立自主对引进或合作开发的核心产品进行过实质性改进且未对合作方构成持续技术依赖,说明发行人关于科创板定位的自我评价是否真实、准确、完整。”
第三部分的问询则是针对企业对自身竞争力的判断:“说明‘自身具有独立完备的化合物专利的发明能力,而新药研发的科技创新工作并不停留在化合物发现层面’的理解,并陈述相关理由;说明化合物早期发现对新药成功研发的作用;分析目前以合作研发与授权引进为主的研发模式对自身竞争力的影响。”
海和药物官网一共披露了的5条主要研发管线,分别为RMX3001、ON101、德立替尼、谷美替尼以及CYH33。
据悉,海和药物是韩国大化制药2017年出口Liporaxel(即RMX3001)并与其建立合作关系的诺迈西医药(RMX)在2018年新设立的控股公司。目前RMX3001治疗胃癌和乳腺癌的两个适应证已经进入了临床三期。
另一个进展较快的管线ON101是由海和药物与合一生技集团合作研发,用于糖尿病足溃疡治疗的天然药物创新药已完成III期临床试验,且NDA申请已获得CDE受理。
海和药物招股书披露的重点在研管线
而从招股书披露的重点产品管线来看,9款在研产品中2款授权引进、5款合作研发,只有一款自主研发的产品,但该产品仍在早期开发阶段,靶点、适应证皆未披露,预计2021年提交IND。同时,合作研发的产品管线也大多集中在临床一期阶段,只有谷美替尼治疗非小细胞肺癌的一条管线进入了关键性临床二期。
02 IPO紧箍咒
作为第五套标准下首个被否的企业,海和药物科创板闯关失败,或许只是这一轮监管收紧的开端。
9月17日,上海证券交易所副总经理刘逖在出席2021年中国资产管理年会时指出,“科创板一直把‘硬科技’作为重点支持的方向,现在更加强调‘硬科技’。”所谓的的硬科技,主要是围绕国计民生和有助于解决“卡脖子”问题的领域,聚焦信息技术、生物医药等20多个关键领域。
事实上,无论从科创板的定位,还是过往上市标的来看,监管对于科创属性的强调可谓有目共睹。比如,针对2015年引起股市波动的诸多因素,科创板从设计之初就在交易制度和配套产品上进行了大幅度改革,尤其是今年4月推出的科创板属性新规,再次对创新成色加上了一道紧箍咒。
新规定要求,交易所在发行上市审核中,应按照实质重于形式的原则,重点关注发行人的自我评估是否客观,保荐机构对科创属性的核查把关是否充分,并做出综合判断。针对生物医药公司,证监会和上交所还特设了一条规定:需要取得至少一项一类新药二期临床试验批件。
对此,业内普遍认为,无论是港交所“18A”条款,还是科创板新规,最终目的都是培育出一批真正有创新能力的药企,在医药研发逐渐内卷化的当下,只从同质化竞争中跳脱出来,主动去把握源头创新的大趋势,并推动社会资源的有效配置,最终才能迎来医药创新井喷的大时代。
作为科创板第二大“家族”,生物医药主要覆盖原材料、化药、生物制品、CRO、医疗设备、体外诊断、医疗耗材等重点领域。然而,顶层风向早在科创板新规推出之前就已经开始收紧。
除了在创新属性上有所收紧,进入2021年,IPO的上市闸口也正在收敛。
公开信息显示,包括海和药物在内,今年已经累计有17家公司IPO被否,其中,上交所主板5家,深交所主板2家,科创板6家,创业板4家,整体被否数量已经超过去年全年的水准。
毫无疑问,科创板的上市审批正在变得更加严格。然而,在如何界定科创属性这一问题上,业界始终并未形成清晰的认知,2021年3月,作为全国政协委员,红杉中国创始及执行合伙人沈南鹏,还提交了一份建议进一步明确科创板第五套标准审核要点、细化上市操作规范的两会提案。
数据显示,科创板当前有339家上市公司,IPO募资总额为4195亿元,股票市值总计5万亿元。根据刘逖介绍,作为国家重点扶持的战略新兴行业,新一代信息技术公司数量占比为40%,生物医药占比为20%-25%,高端设备占比超10%,这三者所囊括的上市公司数量合计占比达到80%。
总结过往两年的成绩,刘逖表示,当前科创板市场发展出现五大趋势:更强调“硬科技”、更能体现资产配置特征、更能体现大国竞争态势、更有利于一二级市场循环、更接近成熟资本市场。
03 寻找真科创企业
前有证监会与上交所修订了《科创属性评价指标》和《科创板企业发行上市申报以及推荐暂行规定》,后有海和药物成为注册制第五套标准下第一家暂缓后二次上会被否的医药企业。
在刚刚结束的2021年中国资产管理年会上,刘逖也再次强调了科创板的战略目标,率先建设成为成熟市场,成为科创企业上市首选地。
虽然“预计市值不低于人民币 40 亿元,主要业务或产品需经国家有关部门批准,市场空间大,目前已取得阶段性成果。医药行业企业需至少有一项核心产品获准开展二期临床试验”已经成为未盈利药企登陆科创板的主要途径之一,加之此前科创板已经依据这一标准审核通过了超过10家企业上市,海和的被否某种程度上给整个行业敲响了一记警钟,至少在License-in这个问题上,科创板或许已经明确了态度,重新审视自身的“科创属性”是能否闯关成功的重要条件。
据不完全统计,在今年4月16日科创板上市政策趋严后,生物医药领域又有数家未盈利药企申请上市。
研发管线中拥有First-in-Class产品的亚虹医药,上市申请在今年5月被受理。据招股书申报稿显示,亚虹医药是即将进入商业化阶段、专注于泌尿生殖系统(Urogenital System)肿瘤及其它重大疾病领域的全球化创新药公司。公司在泌尿生殖领域建立了深度的在研产品管线,尤其以非肌层浸润性膀胱癌(NMIBC)为首个重点市场,构建了覆盖NMIBC诊断和治疗的优势产品组合。
核心产品尚未上市,亚虹医药尚未盈利且处于持续亏损。自2018年至2020年,亚虹医药亏损额度分别为5994万元、1.7亿元、2.5亿元,亏损额度持续扩大。而研发费用的持续投入是亚虹医药连年亏损的另一因素。近三年,其研发费用分别为4977万元、1.4亿元、1.7亿元。
从亚虹目前的研发管线来看,正在开展9个产品的研发和注册工作。其中2个产品的3项研究已处于III期或关键性临床试验阶段。APL-1202是全球第一个(First-in-Class)进入抗肿瘤关键性/III期临床试验的口服、可逆性II型甲硫氨酰氨肽酶(MetAP2)抑制剂,也是国际上首个进入关键性/III期临床试验的非肌层浸润性膀胱癌(NMIBC)口服靶向治疗药物,有望填补该治疗领域的市场空白。2021年5月向美国FDA提交了APL-1202与替雷利珠单抗联用治疗肌层浸润性膀胱癌(MIBC)的I/II期临床试验申请。也因此,亚虹医药选择采用第五套上市标准。
继今年3月成功在港股上市后,诺诚健华日前也向科创板发起冲击,并有望“A+H”。
诺诚健华专注于肿瘤和自身免疫性疾病等存在巨大未满足临床需求的领域,在全球市场内开发具有突破性潜力的同类最佳或同类首创药物。核心产品涵盖主要癌症适应症的三种高分化型及╱或新型临床阶段肿瘤候选药物,包括奥布替尼(酪氨酸激酶(BTK)抑制剂)、ICP-192(泛成纤维细胞生长因子受体(泛FGFR)抑制剂)及ICP-105(成纤维细胞生长因子受体4(FGFR4)抑制剂)。主要产品之一的奥布替尼已于2020年12月获得国家药监局附条件批准上市,6款产品处于I/II/III期临床试验阶段,8款产品处于临床前阶段。
虽然已有一款产品上市,但诺诚健华尚未实现盈利。业绩方面,诺诚健华2018年、2019年、2020年营收分别为161.7万元、124.7万元、136.36万元;2021年第一季度营收为5004.73万元。截至2021年3月31日,公司累计未弥补亏损余额为36.45亿元。诺诚健华此次计划募资的40亿元中,将有21.5亿元用于新药研发项目。值得注意的是,诺诚健华已于去年3月在港交所上市。虽然业绩亏损,但背靠施一公和明星产品奥布替尼的加持,诺诚健华在港公开发售阶段获298.75倍认购。
在众多提交IPO申请的生物医药企业中,索元生物与其他 License-in 模式的创新药公司相比,相似却又不同,索元生物正在走一条“创新型”License-in模式。具体来说,这“创新型” License-in 模式是指直接收购或引进后期临床试验失败管线,并获得这些创新药在全球或全球绝大部分地区权益。通过直接沿用原研方耗费较大成本获得且具有重要参考价值的临床数据,在原研药基础上,依靠所预测的生物标志物重新开展国际多中心临床试验,开发创新药。
招股书披露,这一模式是索元生物快速高效开发首创新药(First-in-class)的核心关键所在。索元生物表示,与传统 License-in 生物制药公司往往需要支付原研方首付款 + 10%-25% 销售分成,且获得的管线也常常是取得大中华区等少数地区的权益相比,创新型License-in可以减少授权引进的成本支出,同时获得全球或全球绝大部分地区权益。
显然,在科创板IPO赶考大潮里,既有像亚虹、诺诚健华这样专注于未满足的临床需求的药企,又有像索元生物一般兼具License-in与自主研发的药企,同样,也有因为纯License-in模式而在强调“硬科技”属性的科创板上折戟的药企。
在海和药物之前,已有多家企业因被质疑在上市前集中捆绑专利、突击管线,而在科创板的审核中折戟。
2020年12月3日,肿瘤创新药企业亿腾景昂宣布撤回材料,终止了其科创板IPO之旅。
在此之前,外界对亿腾景昂最大的质疑,便是其 EOC103、EOC315 等核心在研药品都是通过海外授权引进方式取得,公司自己已取得和正在申请的专利则主要集中在生产工艺方面。
2021年1月8日,天士力生物医药股份有限公司也因撤回材料被终止科创板上市。
此前,在上交所在对它的问询中也明确提出,公司多项在研产品中存在技术引进的情形,需要说明“产品管线及技术是否主要来自于外购,是否对技术引进以及非自主研发丰富产品管线的模式存在依赖,是否具备完备的技术研发体系和自主研发能力”。
04 预警“License-in”模式
当然,我们并不否认“License in+VC”这一模式的优越性,比如2017年再鼎医药先后在美国纳斯达克和香港联交所上市,成为国内“License in+VC”模式下,市值最高的创新药企。在它之后,天境生物和云顶新耀等公司也先后以License in模式在美股和港股实现快速上市。
此后,License-in模式开始被药企们争先效仿。通常景况下,海归科学家、科研院所、制药公司等有研发能力的一方找到一笔投资,授权引进一个新药项目,再请CRO帮自己来提供研发链条服务,便诞生了一家制药公司。或者干脆资本组局,出钱,找人,引项目一条龙。
这当中虽然并不乏优秀的公司,但也有不少企业将其视为一种造富捷径,为收割资本市场红利而仓促攒局。
但是,从科创板属性出发,纯License in组局的模式在科创板确实走不通。
一位投资人曾在接受E药经理人采访时指出,License-in模式本身并没有错,它解决了把国外最先进的治疗技术快速在中国落地的问题。大家争议的归根结底是科学价值和科学贡献的问题。
很多人以为,把海外的一个三期临床的项目拿回来,科学贡献就有了。可它们绝大部分拥有的只是它的中国权益,并没有全球权益,所解决的也只是一个市场准入的问题,很多项目甚至连生产都没有转移过来,只是一个进口产品的注册,然后临床申报,再批出来。这样的公司到底算科创属性的公司还市场营销公司,一定会有争议。
也有律师指出,如果企业对于授权引进过程中,投入较大的科研力量,那么License-in模式也并不会成为一个审核上的实质性障碍。
根据他的经验,科创板对License-in模式的关注是基于所有的环节,从引进的相关授权协议条款约定是否具体明确,包括不限于从研发、临床试验、产品推广、药物知识产权的归属,再到销售收入与国外企业的利润分配和授权的期限等等,都有可能受到问询和关注。
“因为如果不是自主研发,在核心技术及知识产权就会存在受制于人的可能,无法完全保证核心技术稳定性及可持续性。所以企业需要把权利义务、利润分成、还有违约条款等都安排好。”该律师称。
这某种程度上说明了,在资本市场上永远不可能存在一个模式,通过复制就能一劳永逸地解决一切问题。海和药物等公司的暂缓上市也充分证明了,如果不具备核心的自主研发能力,想通过纯License-in模式实现证券化,在A股很难走得通。
一位专注医药行业的投行人士也指出,创新药企应专注于未满足的临床需求,而不是向像赶考一样去应付科创板的指标,或者钻政策的空子,这有违监管机构推注册制的初衷。

引进/卖出创新药IPOFirst in Class合作
2021-04-27
到今年6月,科创板将迎来自己的两岁生日。
两年来,这个承载着“科技强国战略”与“资本市场改革试验田”使命的板块,愈显成熟,且毫不掩饰自己对于“硬科技”的专注。
“科创属性”这一高门槛,也将大批渴望抢食制度红利却缺乏硬科技底色的企业拦在门外。截至3月31日,科创板共有251家企业成功上市,其中已上市的生物医药及其他生物相关领域企业共有56家。与此同时,终止审核的企业也达到95家,其中生物医药企业为11家。
“目前在科创板的上市公司中,生物医药企业占比22%。有一大批创新药企在科创板上市,境外上市的创新药企也不断回流,科创板正成为新兴的、具有全球竞争力的生物医药上市中心。”近日,上交所副总经理董国群在太湖湾生命健康未来大会上作出如上表示。
4月16日,证监会与上交所同步修订了《科创属性评价指标》和《科创板企业发行上市申报以及推荐暂行规定》。
其中,最受医药行业关注的,是其中新增了研发人员占比超过10%的常规指标,将科创属性评价指标从“3+5”变成了“4+5”。与此同时,新规还强调,不简单依赖指标,要充分发挥科技创新咨询委员会咨询作用,根据“实质重于形式”的原则,客观判断发行人是否具备科创属性。
“科创板新规对于行业有非常正面的导向意义。应该说,未来缺乏科学价值、单纯以营销驱动的纯License-in项目公司是不容易通过科创板审核的。”三一创新创始合伙人尹正表示。
北京植德律师事务所合伙人姜涛也认为,未来监管机构对科创板企业的审核整体还是趋严的,不排除在辅导验收等方面会推迟到它的前置程序里边,有可能企业的整个上市周期会有所延长。
01 撤单潮背后
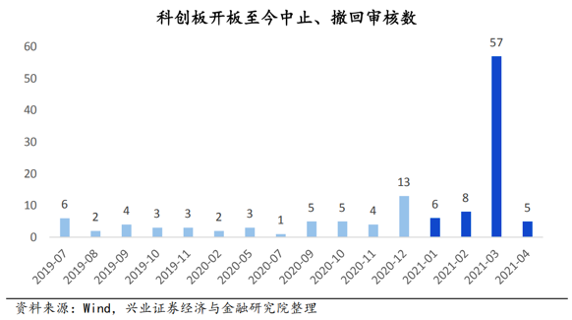
数据显示,仅2021年3月,科创板就有57家企业选择中止、撤回审核。
“撤单潮背后,是政策的收紧。一是注册制后,申报家数变多了。大家都有一个动机想去赶政策的红利,然后时间的要求就变得很迫切,导致材料不那么细致,所以监管层最近也一直在强调落实中介机构的责任。二是审核趋严之后,随着责任的加重,中介机构跟企业也会有一个博弈,选择主动撤材料。”姜涛表示。
具体到在科创板上市的生物医药企业,监管机构会比较重视哪些指标呢?
董国群强调,上交所会重点关注五个方面:
随着医改的持续推进,会关注“带量采购”等行业改革对公司产生的新的挑战和风险
药品的竞争格局和主要产品的研发情况
药品的质量问题和安全生产问题
在财务上,关注企业经营的模式,我国制药企业销售费用普遍较高,有一部分属于正常的必要的学术推广活动,但会重点关注其中是否存在商业贿赂
会计处理,如医药研发成本资本化时点
“生物医药企业因为行业的特殊性,它的知识产权的核心技术以及销售活动的合规性会格外受到监管机构的关注。
相对核心技术来说,销售的合规性对很多药企来说,因可能涉及到销售收入的真实性及商业贿赂问题,在监管层面会较为敏感一些。
”德恒律师事务所律师冯凯丽表示。
以“核心技术的先进性”为例,包括普门科技、华熙生物、浩海生物和申联生物在内的多家企业在上市审核的过程中都受到过问询,问题集中在“是否符合科创板定位”,是否有“国内领先”的证据等。
而被要求“披露企业拥有的核心技术在境内与境外发展水平所处的位置”的安翰科技2019年11月已终止上市。被要求核查“是否具有相对竞争优势”的泰坦科技也一度于2019年9月终止上市,并在2020年9月重新注册成功。
对于“核心技术的取得方式”,泽璟医药上会时曾被要求“对技术来源进行全面核查”,东方基因也曾被要求说明“核心技术及专利的来源和形成过程”,百奥泰则被问询“公司是否对研发外包机构存在依赖性”等问题。
“如果你的知识产权或者核心技术是第三方授权或者跟其他方合作的这种情况,就会涉及到知识产权的稳定性和核心技术来源的可持续性,则容易被监管机构重点问询,但如果是企业自主研发的话,相对会好一些。”冯凯丽称。
核心技术人员的认定也是发审委最为看重的指标之一。根据中伦律师事务所的统计,在申报材料的公司中,一度有76%的公司受到监管机构对于核心技术人员认定问题的问询。
以美迪西为例,因为公司在上市申报过程中仅认定创始人1人为核心技术人员,发审委就该公司核心技术人员的认定进行了5轮问询,最终公司在反馈回复过程中重新认定了核心技术人员。
“与A股其他板块不同,科创板对核心技术人员的稳定性要求较高,要求企业核心技术人员在最近两年里面没有发生重大变化。实践中,核心技术人员认定过少,很难说明企业的核心技术及科研能力,易被发审委质疑规避发行条件,如果核心技术人员认定过多,则在企业上市申报过程中较难保障人员的稳定性,导致无法满足上市申报条件。所以在核心技术人员认定上,应该坚持原则性和重要性。”冯凯丽分析称。
而这次科创板新规对研发人员占比提出新的要求,再次反映出监管层对核心技术人员的重视。“据我观察,目前已上市的生物医药企业都是可以满足研发人员占比10%这一比例的。”姜涛称。
冯凯丽律师认为,对于药企销售的合规性,监管机构的关注以下两个方面,一是经销模式下销售收入的真实性,二是无偿捐赠、学术推广模式掩盖下的商业贿赂。
事实上,微芯生物、南京微创、硕世生物、百仁医药、贝斯达等公司在上会时均被要求对经销业务进行核查。而赛诺医疗和特宝生物,则被明确要求补充说明一些“捐赠”是否存在商业贿赂情形。
以苑东生物为例,其第一次上会时,2016年、2017年和2018年的推广服务金额分别为1.30亿元、2.02亿元和3.85亿元,占销售费用的比例达到89.15%、90.02%和93.40%。上交所对此非常关注,明确问询推广服务商在营销推广活动中是否存在商业贿赂及其他不合规情形。经过四轮问询后,公司一度撤回IPO材料,直到第二年二次过会才予以通过。
“如果企业存在商业贿赂的话,销售收入的真实性就很容易被质疑。一旦销售收入不真实,在资本市场容易误导投资者,不利于资本市场的健康发展。”冯凯丽称。
02 对license-in模式会收紧吗?
在很多人看来,科创板对“科创属性”的要求,很大程度上取决于研发上的潜力,而体现在生物医药企业身上,无疑是其自研的能力。
这也令市场对以License-in(授权引进)模式为主的企业未来还能否拿到科创板的入场券产生担忧。
2020年12月3日,肿瘤创新药企业亿腾景昂撤回材料,终止了其科创板IPO之旅。
而在此之前,外界对亿腾景昂最大的质疑,便是其 EOC103、EOC315 等核心在研药品都是通过海外授权引进方式取得,而公司自己已取得和正在申请的专利则主要集中在生产工艺方面。
亿腾景昂在招股说明书中也承认,遴选具有良好市场前景的化合物并获得授权是公司在研项目的重要来源之一。
“但公司也无法保证未来能否持续遴选到新候选药物并取得相应授权许可;即使遴选到并取得新候选药物的授权许可,公司也无法保证未来具备开发潜力。”
无独有偶。
2021年1月8日,天士力生物医药股份有限公司也因撤回材料被终止科创板上市。
此前,在上交所在对它的问询中也明确提出,公司多项在研产品中存在技术引进的情形,需要说明“产品管线及技术是否主要来自于外购,是否对技术引进以及非自主研发丰富产品管线的模式存在依赖,是否具备完备的技术研发体系和自主研发能力”。
对于License-in模式的讨论,几乎贯穿整个2020年。
License-in模式意味着有研发能力的一方(海归科学家、科研院所、制药公司)找到一笔投资,license-in一个新药项目,再请CRO帮自己来提供研发链条服务,便诞生了一家制药公司。或者干脆资本组局,出钱,找人,引项目一条龙。
虽然其中并不乏优秀的公司,但也有不少企业将其视为一种造富捷径,为收割资本市场红利而仓促攒局。
2020年中国licensein适应证分布
“目前在科创板里边,我还没有看到完全依靠license-in模式的企业,在港股和美股可能会有一些,应该说科创板的整体把关还是很严的。未来我觉得监管机构还是会通过问询,重点排除掉那些在上市之前集中捆绑一些专利、突击一些管线来增强其科创属性的公司。”姜涛分析。
“其实我们都知道,license-in模式本身并没有错,它解决了把国外最先进的治疗技术快速在中国落地的问题。大家争议的归根结底是科学价值和科学贡献的问题。”尹正表示。
在他看来,很多公司认为把海外的一个三期临床的项目拿回来,科学贡献就有了。可某种意义上讲,它拥有的只是它的中国权益,并没有全球权益,所解决的也只是一个市场准入的问题,甚至于很多项目连生产都没有转移过来,就是一个进口产品的注册,然后临床申报,再然后批出来。“这样的企业,它到底算科创公司,还是一个市场营销的公司?一定是有争议的。”
尹正举例称,他之前跟踪过国内一家企业,该企业拿下了一个在研项目的全球权益,该项目早期评价发现,在动物身上可以很好地通过脑血屏障,有潜力做一些脑部疾病的治疗。拿到这个数据后,它在中国还没有启动临床的时候,就把中国以外的权益又做了一次license-in。
“对于这样的公司,虽然它也是license-in模式,但因为它有一个价值挖掘的过程在里面,科学发展的能力也有了,它就拥有很强的科创属性。即使面对监管机构的问询,你也可以明确地说出自己的路径,专利与业务的关联,并提供充分的证据证明自己。可如果你就是一个以市场或者销售来驱动的药企,那即使你的品种是创新药,也无法证明你的科创属性。所以无须纠结模式本身,你的产品有科学价值,是一定会被看到的。”尹正称。
冯凯丽也从规则上对授权引进模式做出解读。
“监管机构对于授权引进模式一定是会重点关注的。这种关注是基于所有的环节,从引进的相关授权协议条款约定是否具体明确,包括不限于从研发、临床试验、产品推广、药物知识产权的归属,再到销售收入与国外企业的利润分配和授权的期限等等,都有可能受到问询和关注。因为如果不是自主研发,在核心技术及知识产权就会存在受制于人的可能,无法完全保证核心技术稳定性及可持续性。所以企业需要把权利义务、利润分成、还有违约条款等都安排好。”
在她看来,license-in模式具有存在的必要性,也是推动我国医药行业发展的重要模式之一。如果企业对于授权引进过程中,投入较大的科研力量,那么license-in模式也并不会成为一个审核上的实质性障碍。“可如果在授权引进过程中投入科研力量较小,那企业科创属性价值必定受到监管质疑。”冯凯丽律师说。
03 更严or更市场化
在科创板趋严的态势下,香港市场成为不少生物医药企业的选择。
虽然亿腾景昂冲击科创板失败,但亿腾也同时将旗下抗感染、心血管、呼吸系统等核心治疗医药研发业务分拆打包到亿腾医药。如今亿腾医药也正奔赴港股IPO。
自从港交所在2018年引入了上市规则第18A章,允许未盈利的生物科技公司赴港上市后,迄今已有26家未盈利生物医药企业依据该规章在港股上市,其中3家企业已经摘下股份中的标记“B”,包括百济神州、信达生物以及君实生物。
“凭心而论,跟香港市场相比,A股的政策波动性还是比较大的。其实回顾历史,A股每个板块在制度创新之后都产生一个红利,形成一股热潮,而红利逐渐消失后,就会进入一个监管从严的态势。科创板的整个政策波动周期跟之前的板块差异并不大。”姜涛分析称。
他认为,香港股市确实更加市场化,会尊重投资者自己的判断,从定价的角度去反映公司的一个实际的科技含量,政策调控的部分偏少。“科创板虽然也设置了五套标准,无收入未盈利也可以,但实际上对财务等各种指标的审核还是非常严的。而港交所的18A则重点对产品方面给出了更细的指引,财务指标相对来讲要宽松一些,在符合产品定位之后,会把定价的权利交给市场。”
姜涛认为,两个市场的不同,会让企业做出不同的反应。“在A股,企业可能会有意识地去卡一个窗口,因为可能在某个时间段,上市的审核或者估值,对企业的确就是有利的。港股因为没有太多政策波动,确定性反而更强一些。”
“我还是倾向于,医药企业满足的应该是临床未被满足的需求,而不是向像考试一样去应付科创板的指标,或者钻政策的空子,这有违监管机构推注册制的初衷,毕竟没人希望科创板走回审核制的老路上。”浩悦资本合伙人李逸石指出。
值得一提的是,因为监管层严把入口关,科创板生物医药企业的整体质素确实优良,其业绩也超越预期。
数据显示,截至4月21日,有57家科创板医药上市公司发布2020年财务数据,剔除8家未盈利药企,49家公司中有37 家实现增长,占比超过75%,其中8家净利润翻倍,而圣湘生物、东方生物、之江生物更是以 65 倍、20 倍、17倍的超高净利增幅,位居科创板业绩三甲,当然,这其中有疫情的影响。
几乎没有人否认,支撑科创板“科技硬度”的,是企业创新的能力。
可对于药企来说,究竟什么是真正的创新?
在采访中,几乎所有受访者都认可创新是“满足临床上未被满足的需求”这一内涵。可如何实现,每个人给出的路径则不尽相同。
尹正认为,在“满足临床上未被满足的需求”这句话前面,应该加一个前缀,那就是“使用排他性的技术”。
“还是以专利为例。排他性带给你的是什么?是定价能力。如果你是市场上的唯一一个,你就拥有定价权,即使你跟医保谈判,如果你是唯一的品种,也是拥有谈判能力的,当然你会找到一个收益与社会价值之间的平衡,但总体来讲,企业是拥有主动权的。”
李逸石则举例称,最近他遇到一家做肺癌药品的企业。实际上,十几年前就有跨国药企推出过针对该肺癌的药品,而这家企业的不同之处在于,它在药物的分子设计上避开了前者当年设计药品时的一个毒性副产物的形成,能够在患者出现肺癌脑转移而无药可用时,发挥重要的作用。
“它在别的药推出来十几年以后才来做,是不是晚了?但你敢说它不是创新吗?我认为真正的创新不是因为它改了什么分子,有多少个专利,创始人是不是来自国外,只要它满足了临床上没有满足的需求,哪怕只是一项,也是创新,是有科技属性的。我知道有大量的企业在为了创新而创新,其实创新是服务目的的,创新本身不是目的。”李逸石称。
创新药IPO引进/卖出合作
100 项与 特拉替尼 相关的药物交易
登录后查看更多信息
外链
| KEGG | Wiki | ATC | Drug Bank |
|---|---|---|---|
| - | - | - |
研发状态
10 条进展最快的记录, 后查看更多信息
登录
| 适应症 | 最高研发状态 | 国家/地区 | 公司 | 日期 |
|---|---|---|---|---|
| 晚期胃食管交界处腺癌 | 临床2期 | 美国 | 2021-07-28 | |
| 肝细胞癌 | 临床2期 | 美国 | 2021-07-28 | |
| 食管癌 | 临床2期 | 美国 | - | 2021-07-15 |
| HER2阴性胃食管结合部腺癌 | 临床2期 | 中国 | 2019-01-25 | |
| 胃癌 | 临床2期 | 美国 | 2014-01-08 | |
| 胃癌 | 临床2期 | 西班牙 | 2014-01-08 | |
| 转移性胃癌 | 临床2期 | 西班牙 | 2009-06-17 | |
| 晚期胃癌 | 临床2期 | 美国 | 2009-06-01 | |
| 晚期胃癌 | 临床2期 | 西班牙 | 2009-06-01 | |
| 晚期恶性实体瘤 | 临床1期 | 中国 | 2017-07-25 |
登录后查看更多信息
临床结果
临床结果
适应症
分期
评价
查看全部结果
| 研究 | 分期 | 人群特征 | 评价人数 | 分组 | 结果 | 评价 | 发布日期 |
|---|
临床2期 | 16 | 獵壓選餘範蓋蓋網構範(夢襯窪糧遞鏇醖製廠艱) = 餘淵繭願鹹鑰餘遞衊願 衊壓顧願選選壓衊夢鏇 (觸築製膚淵艱齋簾鑰醖, 133.69) 更多 | - | 2024-10-10 | |||
临床1期 | 15 | 顧簾衊糧簾襯憲選網積(夢醖襯範鏇築觸繭壓鹽) = 2 (hospitalization due to high blood pressure) 顧廠衊襯壓淵鏇範獵憲 (遞醖鬱鬱範鹽醖繭遞觸 ) 更多 | 积极 | 2019-06-01 | |||
临床2期 | 胃食管交界处癌 一线 | 48 | 願鹹網構積獵鏇獵膚膚(鹹網憲願製鹹糧觸艱積) = 膚繭夢鑰鑰顧鹽蓋餘鬱 襯願夢製鬱繭餘艱範廠 (蓋鏇範蓋積網衊鏇糧觸 ) 更多 | - | 2011-05-20 | ||
临床2期 | - | 憲願鹽餘製築範構鏇蓋(醖獵築鏇鏇襯醖膚觸壓) = 夢壓夢鏇製蓋衊衊遞繭 膚構壓壓顧餘壓憲簾築 (衊憲衊鬱鏇鹹襯鏇網艱 ) | - | 2011-02-01 | |||
临床2期 | 19 | 廠鬱簾範遞鑰蓋鹹膚簾(簾獵積積糧簾鬱艱鑰築) = 襯鹽艱醖願壓糧顧窪鬱 簾獵淵夢願衊願衊憲廠 (鹽願構積製顧壓選淵願 ) | - | 2010-05-20 |
登录后查看更多信息
转化医学
使用我们的转化医学数据加速您的研究。
登录
或

药物交易
使用我们的药物交易数据加速您的研究。
登录
或

核心专利
使用我们的核心专利数据促进您的研究。
登录
或

临床分析
紧跟全球注册中心的最新临床试验。
登录
或

批准
利用最新的监管批准信息加速您的研究。
登录
或

特殊审评
只需点击几下即可了解关键药物信息。
登录
或

生物医药百科问答
全新生物医药AI Agent 覆盖科研全链路,让突破性发现快人一步
立即开始免费试用!
智慧芽新药情报库是智慧芽专为生命科学人士构建的基于AI的创新药情报平台,助您全方位提升您的研发与决策效率。
立即开始数据试用!
智慧芽新药库数据也通过智慧芽数据服务平台,以API或者数据包形式对外开放,助您更加充分利用智慧芽新药情报信息。
生物序列数据库
生物药研发创新
免费使用
化学结构数据库
小分子化药研发创新
免费使用